-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Production of Lithium-Ion Batteries
Publication
PFAS – Rougher Waters Ahead?
Publication
Generative Artificial Intelligence in Insurance – Three Lessons for Transformation from Past Arrivals of General-Purpose Technologies
Publication
Did you Know? A Brief Reflection on La Niña and El Niño
Publication
Time to Limit the Risk of Cyber War in Property (Re)insurance -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
Fasting – A Tradition Across Civilizations
Publication
When Actuaries Meet Claims Managers – Data-Driven Disability Claims Review Business School
Business School
Publication
Chronic Pain and the Role of Insurers – A Multifactorial Perspective on Causes, Therapies and Prognosis
Publication
Simplicity, Interpretability, and Effective Variable Selection with LASSO Regression Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Eye Spy – A Closer Look at the Management of Visual Impairment Claims

December 27, 2015
Mary Enslin
English
Introduction
The human eye is a highly sophisticated organ with many intricate parts that, under normal circumstances, work together to create sight. As a result of the eye’s complex anatomy, numerous disorders can affect the organ; these can be caused by genetic abnormalities, congenital problems, disease, trauma or ageing. The results can be temporary, as in the case of short-term infections, or permanent with potentially life-changing consequences. There can be no arguing that the impact of vision loss is multi-dimensional, with personal, social, psychological and economic consequences.
But how common is visual disability and what is the impact on the lives of those affected? This article will examine the extent of visual disability globally and discuss how it may have an impact on insurance claims, especially those related to Disability, Critical Illness and Long Term Care products. Some of the challenges facing claims assessors are also discussed.
Definition
Visual impairment can be described as any chronic visual deficit that impairs everyday functioning. It can range from mild to severe and includes functional and total blindness. While the precise diagnosis is vital for determining the treatment course and prognosis, the most important element of any eye disorder is the effect it has on vision.
Many factors comprise an individual’s visual capacity, including: depth perception, visual motor ability, visual perception, colour perception, the ability to perceive contrast, etc. However, most medical experts agree that the two most influential factors on one’s ability to see are visual acuity and visual field.
- Visual acuity is defined as a measure of central vision, the ability to distinguish details and shapes of objects. This is most frequently measured using a Snellen chart producing a fraction-type score.
- Visual field describes the entire area that a person is able to see when their eyes are fixed in one position. It is usually measured in degrees using perimetry or campimetry, whereby the patient must detect the presence of defined targets on a test background (i. e. identify white dots as they become visible).
These factors are so important that they are central to most legal definitions of blindness. For example, the World Health Organisation (WHO) defines blindness as “visual acuity less than 6/60 (20/200), or a corresponding visual field loss less than 20°, in the better eye with the best possible correction”.
Epidemiology and causes of visual impairment
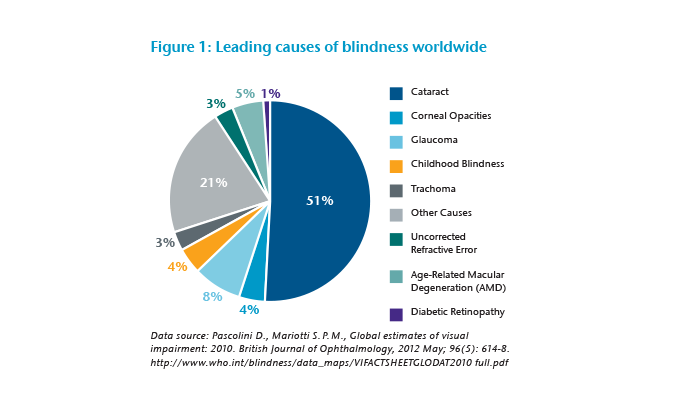
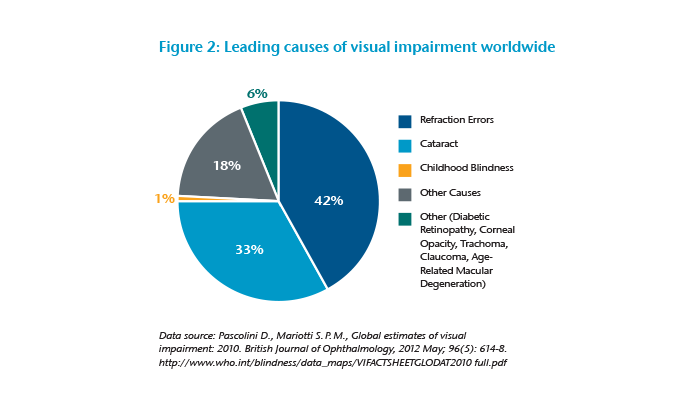
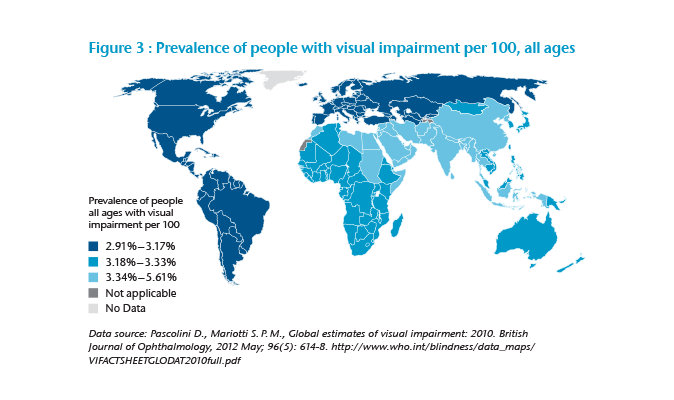
WHO estimates that 285 million people are affected by some form of visual impairment (severe to moderate) worldwide, approximately 4.25% of the global population. Of these, 39 million (14%) are described as blind. Globally, uncorrected refractive errors are the main cause of visual impairment, followed by cataracts and glaucoma, while cataracts, glaucoma and age-related macular degeneration are the leading causes of blindness. Diabetic retinopathy is also a significant cause of visual impairment.
These estimates account for all ages; thus, children and the elderly are included; however, a significant portion of eye-related conditions occur with ageing. In fact, WHO estimates that people over the age of 50 years account for as many as 82% of all blind people. Considering the increasing epidemics of diabetes and other chronic diseases, and the rapidly ageing population, it is expected that the number of blind people will grow significantly in all regions – unless action is taken to prevent and cure the main causes of visual impairments.
For our purposes it is important to consider the effects of visual impairment on the potential insurable population. The data presents a number of challenges as many studies do not differentiate according to age and socio-economic status when estimating prevalence. Furthermore, the causes of visual impairment may differ in the working-age population. For example, the majority of visual impairments in people younger than 40 years are caused by refractive errors and accidental eye injury, with more than half of all patients treated for eye injuries aged 18 to 45 and almost 30% of these between 30 to 40 years old.
Diabetic retinopathy also affects this age group significantly and is the leading cause of blindness among the working-age population. Approximately 11% of Americans who have diabetes and are age 20 years or older also have some form of visual impairment, and this is expected to worsen as the diabetes epidemic grows. In fact, one source suggested that the number of people who experience diabetic retinopathy is expected to triple from 2005 to 2050, from 5.5 million to 16 million.
Considering variances in the data, a best estimate would indicate the number of adults who are age 15 to 49 and affected by visual impairment is just over 80 million, approximately 2.26% of the adult population.
Treatment and prognosis
As one would imagine, any specific treatment plan and prognosis depends heavily on the individual diagnosis. However, it is of significance that as much as 80% of visual impairment is thought to be avoidable through prevention or cure. The statistics are particularly poor in countries with poor health infrastructure and overall poor economic development. In fact, around 60% of the world’s blind people live in sub-Saharan Africa, China and India. However, there are still many causes of vision loss for which there are no cures.
Another factor to consider when thinking about treatment and prognosis is that people with vision loss are more likely to experience certain comorbid conditions than those with normal vision; for example, the risk of depression is three times higher and the risk of falls increases two times. The visually impaired population is also at greater risk for hearing impairment, heart disease, stroke, cognitive decline and premature death.
One also needs to consider that the effects of these comorbid conditions may be more disabling when compounded with a visual impairment, compared to a claimant with a single diagnosis alone. A further consideration is the effect visual impairment will have on life expectancy. Some studies have found that the blind have an age-specific mortality three to seven times greater than the general population.

Given that many visual impairments are preventable, it is important to ensure that claimants receive optimal treatment prior to any decision being made regarding permanence. The treating specialist will be in the best position to comment on this, although an independent medical examination by a specialist – an Ophthalmologist, an Occupational Therapist or a Visual Rehabilitation Specialist – will provide valuable insights. Further, discussions with the chief medical officer and referral to the reinsurer may also be helpful.
Once it has been established that the claimant has reached Maximum Medical Improvement (MMI), and a degree of visual impairment remains, then it is important that the claimant undergo a visual rehabilitation programme. The goals of such a programme are not to restore sight, as one would assume all options in this regard would have been explored, but rather to restore functional ability and improve quality of life and independence. Elements of a successful visual rehabilitation programme include:
- Emotional and intellectual preparedness
As mentioned, depression is a common issue and programmes need to address the emotional needs of the claimants and their families to assist them in accepting this change in their lives. - Learning skills and alternative techniques for independence
- Mobility training (i. e. long-cane travel, use of guides)
- Communication skills, including Braille if appropriate
- Typing and computer use
- Home making (i. e. home maintenance, chores, cooking, etc.)
- Grooming/self-care skills
- Socialisation skills
- Provision of appropriate adapted or special equipment
- Permanent or temporary (i. e. magnifiers)
- Technology, including numerous apps and gadgets for those with visual impairment
- Adaptations to the environment
It will be important to discuss what accommodations can be made in the home and workplace to allow for independence and return to work. - Education and promotion of employment capabilities to employers
- Reskilling, training or further education (where needed)
Those who cannot return to work in their own occupation (i. e. work activities are too demanding or dangerous, or health and safety regulations do not allow for accommodations) may benefit from further education or reskilling. Available programmes differ per region but there are many organisations that offer online courses or can direct you to local training opportunities. See http://www.hadley.edu. - Vocational training and work hardening
- Address any other significant comorbid diseases or disabilities
- Support network
- Mentoring
- Family involvement
Claims considerations
Consider these three facts regarding moderate to severe visual impairments: they occur predominantly in developing countries where the population is unlikely to have disability insurance; they most commonly affect those over the age of 50; and they only appear to affect 2%-3% of working-age adults. With those facts in mind, one might ask whether visual impairment is of relevance to the insurance industry.
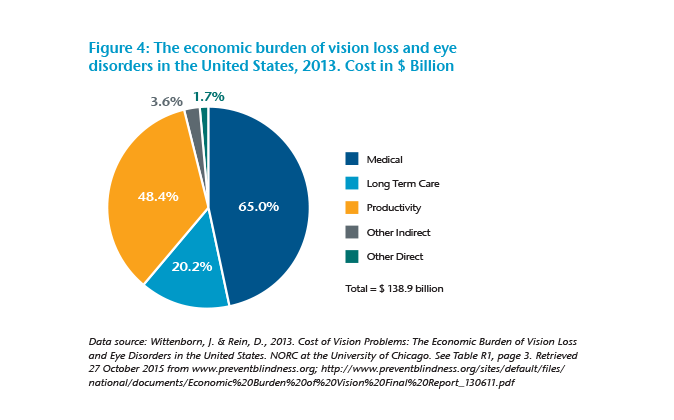
Despite the above, visual disability remains one of the top 10 disabilities among adults 18 years and older. Furthermore, if not managed correctly, it can result in life-long debilitating disability with significant financial implications.
Estimates of the cost and economic impact of visual impairment vary greatly by source and method of measurement. One study using 1993 data estimated that the annual worldwide productivity cost of blindness was $ 168 billion, while another study based on the American population indicated the productivity cost alone was $ 48.4 billion (excluding other indirect expenses). A 2011 Deloitte Access Economics study estimated the financial cost of vision impairment in Ireland as € 386 million – 43% of which is due to lost productivity (employment). This is expected to increase to € 449 million by 2020 (in real terms). Thus one could argue that while the number of visual impairment claims is few, the potential costs to the insurer may be significant.
Furthermore, visual disability claims present a unique set of challenges to claims assessors:
A. Jargon
Visual disability claims are frequently complex, and technical and claims assessors may not feel confident understanding the jargon and test results used by healthcare and rehabilitation specialists reporting on ocular diseases and visual impairments. We have compiled a quick reference list of the most commonly used jargon/shorthand in ophthalmology to assist assessors with this. Further, the opinion of the chief medical officer or an independent specialist may be useful, particularly in rare or complicated diagnoses.
Common jargon
cC – With correction (i. e. with glasses).
sC – Without correction.
CF – Counting fingers, this method of testing visual acuity is used when it has been determined that the patient is unable to make out any letters or shapes on the acuity chart. For example, CF 5’ or CF 1.5 m would indicate that the patient can count the examiner’s fingers from a maximum distance of 5 feet or 1.5 metres.
D – Diopter, a unit used to designate the refractive power of a lens. In vision correction an Optometrist may prescribe glasses with a power of -1.00 D to -3.00 D (in myopia) and +1.00 to +3.00 (in hyperopia).
HM – Hand motion, a method used only if the counting fingers method yields little or no success. The examiner records the patient’s ability to distinguish whether there is movement of the examiner’s hand directly in front of their eyes.
LASIK – Laser in Situ Keratomileusis, a type of refractive surgery in which the cornea is reshaped to change its optical power. Used for correcting myopia, hyperopia, astigmatism.
LogMAR – Logarithm of the minimum angle of resolution, an alternative expression of visual acuity. It measures visual acuity loss; hence, positive values indicate vision loss while negative values denote normal or better visual acuity.
LP/NLP – Light perception/no light perception, an indication of the patient’s ability to perceive any light.
OD – Right eye (oculus dexter).
OS – Left eye (ocular sinister).
OU – Both eyes (oculus uterque).
PEARL – Pupils Equal And Reactive to Light.
Perimetry or Campimetry – A method for testing visual field whereby the patient must detect the presence of defined targets on a test background (i. e. identify when white dots become visible).
Phacoemulsification – The use of ultrasound vibration to shatter and break up a cataract, making it easier to remove.
Snellen Chart – Most common eye chart; used to measure visual acuity.
Snellen Fraction – A representation of visual acuity in the form of a fraction: visual acuity = distance at which test is made (measured in feet or metres)/distance at which a person with “normal” vision would theoretically discern the same letter or shape. In many countries it is normal to write this fraction as a decimal: 6/6 = 20/20 = 1.
VA – Visual Acuity, a measurement of the eye’s ability to distinguish object details and shape, usually measured with a Snellen chart and described using a Snellen fraction.
VF – Visual Field, the full extent of the area visible to an eye that is fixating straight ahead.
B. Availability of resources and treatment
As mentioned, a significant percentage of visual impairment is preventable if treatment is sought in a timely way. Unfortunately, a lack of awareness often results in at-risk individuals failing to go for preventative visual screening and/or seeking treatment too late. From a claims perspective, it is important to ensure the claimant is receiving optimal care, and products such as permanent (lump sum) Disability and Critical Illness should only be assessed once MMI has been established.
However, it is important to take into account what treatment can be considered reasonable by the insurer. Many claimants may decline to undergo surgery, even when this is indicated as possible treatment for their condition. Given the number of risks associated with any surgery, and further that any surgery to the eye has its own added risks, it is not reasonable for an insurer to insist that a claimant pursue this course of treatment. This may be true of other experimental treatments with high associated risks or poor success rates.
Thus, when determining whether MMI has been reached, and the effect of any residual impairment, it may be useful to consider the following:
Has the diagnosis and degree of permanent visual impairment been verified by a specialist? This should be based on more than a Snellen test alone as it is easy to manipulate these results.
- Has the claimant completed a comprehensive visual rehabilitation programme with elements described above?
- Can any aspects of the claimant’s work be adapted using technology or assisted by someone else (i. e. role sharing), and is the employer willing to make accommodations? Bear in mind that in some countries the provision of reasonable accommodations is required by law.
- Do any licensing issues preclude the claimant from some or all work duties? I. e. driver’s license, health and safety medical certificate (e. g. mining industry), etc.
- If the claimant cannot be accommodated in his/her previous occupation, what retraining opportunities are available?
- Does the policy allow for a partial benefit or rehabilitation benefit to cover the initial expense of adaptations and accommodations, thus allowing an individual to continue working? For example, special transportation arrangements to work, visual and sensory aids, attendant care services, service animal expenses (if relevant).
For Critical Illness policies, if blindness is covered, one needs to examine the exact definition. Many policies have vague wording requiring “total loss of vision” without specifying if this is functional vision, legal blindness, light perception, one eye or both, etc. We would strongly encourage product developers to make definitions as detailed as possible to avoid confusion at claims stage. However, if this is unavoidable, market practice will dictate the approach that is used. It is important for claims assessors to remember that many people experience functional limitations due to vision loss but do not meet the criteria for legal blindness.
For Long Term Care products, assessors need to bear in mind that individuals with visual impairment are at greater risk of comorbid illnesses and on average are admitted to nursing homes three years earlier than the general population. They are also twice as likely to require the use of health services or hospitalisation and stay twice as long in hospital. This may have implications for claims management.
C. Preconceptions, attitudes and beliefs
Every individual has his/her own preconceived ideas about the capabilities of those with moderate to severe loss of vision. However, many of these are based on unreliable sources (e. g. movies or television) and limited personal experience.
In many cases permanent disability can be avoided and many advocates suggest that there are very few occupations that cannot be successfully executed by people with visual impairments. To quote the National Federation of the Blind, “Given proper training and opportunity, the average blind person can do the average job in the average place of business, and do it as well as his or her sighted neighbor.” And yet a 2015 study found that only 40% of working-age adults (age 21 to 64) were employed in the USA, regardless of education level. Similarly, in 2012 the UK government reported that just over half (52%) of all visually impaired applicants qualified for some degree of financial aid, while only 47% were found fit for work. Of course, in countries where infrastructure and work opportunities are not as developed or supportive, the percentage of people unable to work due to visual impairment can be even greater, with some estimating as many as 90% of blind individuals being unable to work.
Considering the varying levels of functional performance, even among individuals with the same degree of visual impairment, it is clear that attitudes and perceptions play a significant role in determining the level of independence achieved. However, it is not only the attitudes of the affected individuals that have an influence, but also the attitudes of family and friends, treating medical professionals and even claims assessors.
Conclusion
Claims assessors cannot be expected to be experts in all aspects of visual performance and we often need to rely on the opinion of experts in this field. However, familiarizing yourself with the jargon, treatment options, rehabilitation benefits and workplace accommodations available in your market will assist greatly with accurately assessment and managing claims. While visual impairment is a life-changing event, it certainly does not mean the end of independence and economic activity. It is important to remember that with proper rehabilitation, accommodation and support, individuals with visual impairment can continue to live meaningful lives and contribute productively to society. The following case studies illustrate some of the challenges discussed in this article and highlight necessary considerations when assessing visual impairment claims.




