-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Florida Property Tort Reforms – Evolving Conditions
Publication
Is Human Trafficking the Next Big Liability Exposure for Insurers?
Publication
When Likes Turn to Lawsuits – Social Media Addiction and the Insurance Fallout
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Understanding Physician Contracts When Underwriting Disability Insurance
Publication
Voice Analytics – Insurance Industry Applications [Webinar]
Publication
GLP-1 Receptor Agonists – From Evolution to Revolution U.S. Industry Events
U.S. Industry Events
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Chronic Fatigue Syndrome – Challenges in Claims Assessment

February 27, 2025
Johannes Schmidt
Region: Germany
English
Deutsch
A lot has been said surrounding the topic of chronic fatigue syndrome (CFS). We hope to shed some light on the background of the disorder and provide claims assessors with valuable tips for their reviews of long-term disability (LTD) claims. Although we are pulling our knowledge from LTD claims in Germany, we know the learnings could be valuable to all.
Definitions
In occupational disability claims, terms such as tiredness, exhaustion, chronic fatigue, chronic fatigue syndrome (CFS), and post-COVID‑19 are often mentioned. However, these terms are not synonymous. Let’s clarify the differences.
Fatigue (from Latin: fatigatio) generally refers to a disproportionate and subjectively perceived exhaustion that occurs regardless of stress levels and does not significantly improve with rest or sleep. This kind of exhaustion might be a symptom of a wide variety of disorders and can occur, for example, as part of treating a cancerous tumour, rheumatic disorders, multiple sclerosis or CFS.1
CFS itself is generally considered to be a serious and often chronic disorder characterized by fatigue among several other symptoms, including sleep issues, cognitive impairment, pain, and orthostatic intolerance. However, the main symptom is exertion intolerance, abbreviated as post-exertional malaise (PEM). PEM refers to a worsening of the overall symptoms that can manifest as fatigue, in severe cases often after the slightest physical, mental or psychological exertion such as walking, brushing teeth, stimulus overload or having conversations.2
There are several synonyms for CFS, including “post-viral fatigue syndrome” or “myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)”. Another term is “systemic exertion intolerance disease (SEID)”, but this has not yet become established in general usage, even though it is less misleading and emphasises the main symptom of PEM.
CFS was included in the International Statistical Classification of Diseases (ICD) as a neurological disorder in 1969 (ICD‑10: G93.3). The COVID‑19 pandemic has brought CFS back into the spotlight, since many people affected by post-COVID also suffer from symptoms such as chronic fatigue. It is important to note here that long COVID and post-COVID are not the same as CFS but are summarised as a wide variety of health complaints that are difficult to distinguish. These usually persist for more than one month (in the case of long COVID) or three months (in the case of post-COVID) after a SARS‑CoV‑2 infection and cannot be explained in any other way.
This does not necessarily mean that a person experiencing these symptoms meets the criteria for CFS. Thus, the circular argument that post-COVID patients automatically suffer from CFS is incorrect.
Let’s look at some common myths surrounding the topic of CFS.
Myth 1: CFS Can be Diagnosed by a (Laboratory) Test
Even if a (laboratory) test would simplify the disability claims management process, it should be noted that despite ongoing research a clear objective marker for diagnosing CFS has not yet been identified.
Sometimes, disability claims contain reports from “specialised laboratories” with unusual results, especially on specific autoantibodies, suggesting that CFS has been detected. However, without a generally accepted etiopathogenetic concept,3 these remain experimental scientific approaches that are neither falsifiable nor lead to a definitive diagnosis, let alone provide evidence for the reported functional impairments. Laboratory tests are primarily used for the differential diagnosis of suspected CFS and to identify comorbidities and deficiencies. Generally, institutions that describe themselves as “specialized laboratories for CFS” or “specialized experts in fatigue” should be approached with caution – if you want to know more about this, we recommend you take a look at a German paper by Dreßing and Dreßing (2024)4 which emphasises the necessity of sufficient specialist knowledge, experience, and further training in the relevant area of law.
An expert’s first step when conducting an IME (independent medical examination) or within the claims management process is to take a comprehensive medical history to record the specific complaints and impairments of the insured person in detail. Questionnaires and symptom diaries can also be useful tools. It is important to inquire about the level of functioning in daily life and to clarify the symptoms over time, rather than just as a snapshot. If a suspected CFS symptom is attributed to a SARS‑CoV‑2 infection, it is important to review the medical history for the period before the infection to check for possible alternative explanations and assess the pre-morbid level of functioning.
The Canadian Consensus Criteria (CCC)5 – as one of several available diagnostic criteria – provide strict but widely accepted criteria for the diagnostic classification of CFS. A medical examination is required to determine whether these criteria are met. Accordingly, the primary symptom of PEM, along with fatigue, symptoms from the categories of pain, sleep disorders, neurocognitive symptoms and other symptoms must persist for at least six months (three months for children and adolescents). See our simplified overview.
Clinical Features of CFS (Simplified Self-created Representation Based on the CCC)
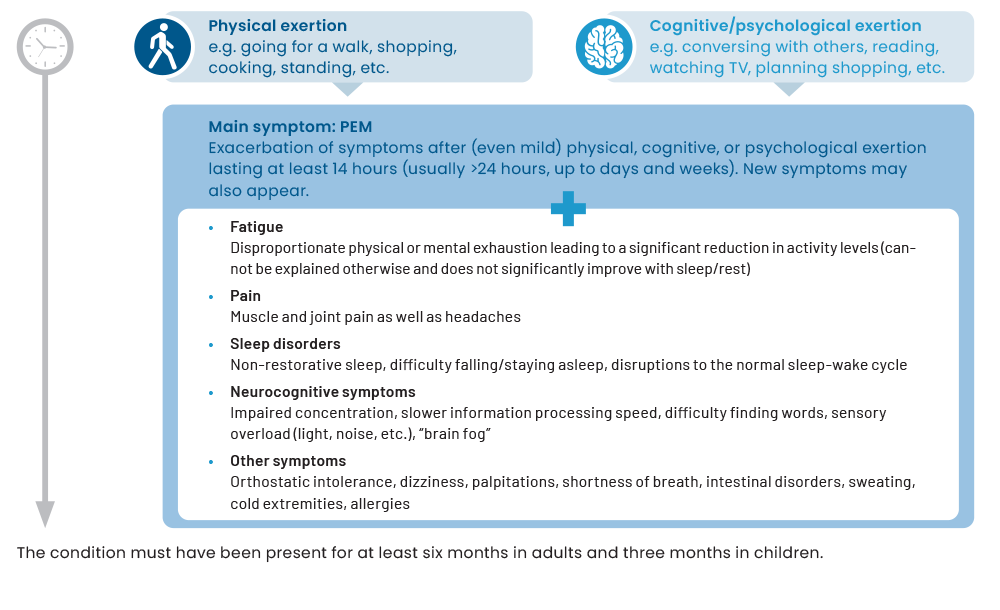
The main symptom of CFS is therefore PEM, which typically occurs from a few hours after an exertion to up to three days later. The duration can vary from individual to individual and may last hours or even weeks; a worsening of symptoms for a minimum of at least half a day to a whole day is to be expected according to the CCC.6
Although it is not an objective marker, one possibility for checking the plausibility of exertion intolerance and muscular fatigue could be measuring the handgrip strength.7 In this test, hand strength is measured 10 times in succession using a hand dynamometer; this procedure is then repeated after one hour. Typically, the hand strength of CFS patients decreases within a series of measurements, and does not return to its baseline level during the repeated measurement after one hour. These results are an indication of exertion intolerance and persistent muscular fatigue. Due to the repeated measurement, the result is difficult to falsify subjectively.
There are other tools that can help to verify different symptoms of CFS; even though these are not objective markers either. Aside from neuropsychological testing in cases of reported cognitive impairment, orthostatic intolerance that occurs in around two thirds of CFS patients should be mentioned here.8 Orthostatic intolerance means the inability to adapt the circulation to an upright position, so that patients cannot stand or sit for long periods and may complain of vertigo, dizziness, tachycardia, fluctuations in blood pressure, balance problems or pallor, among other symptoms. These improve when the patient is lying down, which explains why many CFS patients spend a large part of their day in bed.
One form of orthostatic intolerance is called postural orthostatic tachycardia syndrome (POTS), which can be determined using the NASA lean test, without the need for special equipment.9 In the NASA lean test, the patient lies down for a few minutes before pulse and blood pressure are measured twice to determine the resting heart rate. Afterwards the patient leans with the shoulders slightly slanted against a wall. Then blood pressure and pulse are measured every minute for 10 minutes.
The test is positive if there is an increase in heart rate of more than 30 beats per minute (children and adolescents: 40 beats per minute) during the 10‑minute standing period or if the heart rate continues at more than 120 beats per minute. If a sustained drop in blood pressure of >20mmHg systolic and/or >10mmHg diastolic is detected when standing, orthostatic hypotension is also present – this refers to a type of low blood pressure where the blood pressure drops sharply shortly after standing up from a lying or sitting position. If the result of the test is positive, it is advisable to verify the presence of orthostatic intolerance with a tilt table test. However, one needs to have the appropriate equipment for this, namely a tilt table.
Preliminary Conclusion
Although the myth that there is a specific test, an objective marker or a laboratory test to diagnose CFS is incorrect, different tools are available and can be helpful to make CFS-symptoms plausible. See our summary of the most important diagnostic tools for the diagnostic questions relevant to CFS, focused on assessing a person’s functional capability.
Diagnostic Toolbox For CFS Based on Hoffmann et al. (2024)10
|
Subject of investigation |
Diagnostic tool |
|---|---|
|
Review diagnostic criteria |
Criteria catalogues e.g:
|
|
Severity and frequency of CFS symptoms |
|
|
Subjective severity of fatigue |
|
|
Subjective severity of PEM |
|
|
Severity of the functional impairment |
|
|
Sleep disorders |
|
|
Muscular fatigue |
|
|
Orthostatic intolerance (e.g. postural orthostatic tachycardia syndrome (POTS) or orthostatic hypotension (OH)) |
|
|
Cognitive impairments |
|
In addition to the tests mentioned, behavioral observation and clinical impressions (combined with a preliminary physical examination) play an important role. The following is a non-exhaustive list of other symptoms that may be observed in some CFS patients:
- Painful lymph nodes
- Tachycardia
- Fluctuations in blood pressure
- Extreme pallor
- Sweating
- Cold extremities (cold hands or feet)
- Weight changes
- Muscle atrophy
- Tiredness and the tendency to exhaustion during an examination
- Difficulty with finding words or other cognitive problems become apparent
- Poor general state of health
- Psychologically burdened
It should be emphasised that a diagnosis of CFS should not be made too early or too hastily. Instead, a diagnosis should be made only at the end of a comprehensive and interdisciplinary differential diagnosis, in which the following diagnoses in particular should be taken into account:11
- Chronic infections such as hepatitis or Lyme disease
- Thyroid disorders such as Hashimoto’s thyroiditis, hypothyroidism, hyperthyroidism
- Autoimmune disorders such as rheumatism
- Tumour diseases
- Cardiovascular disorders such as heart failure
- Neurological disorders such as multiple sclerosis, small fibre neuropathy
- Restless legs syndrome
- Sleep disorders such as chronic insomnia, obstructive sleep apnoea
- Gastrointestinal disorders such as coeliac disease or Crohn’s disease
- Mental disorders such as depression or somatoform disorders
Examining all theoretically possible differential diagnoses is not viable; instead, the focus should be on the main symptoms. If, for example, a young woman with unexplained thyroid values complains of severe fatigue and weight gain without an obvious cause, Hashimoto’s thyroiditis should be considered and investigated in the laboratory.
If a patient reports psychological complaints, these should also be investigated – along with the question of whether they are a result of a possible CFS condition. This should be carefully considered because it’s not only CFS, but also depression, for example, that can be accompanied by tiredness and exhaustion. However, depression is different from CFS in that CFS does not usually involve a lack of motivation and drive. CFS patients usually want to be active, but overexertion (e.g. through sport) is associated with a worsening of the condition – while people who are depressed generally benefit from being more active, but often lack the drive to do so.12
Conclusion
There is no specific test to detect CFS but a variety of diagnostic tools are available that can be helpful identifying typical symptoms of CFS. The diagnosis of CFS should not be made prematurely, but only after comprehensive differential and exclusion diagnostics that focus on the main symptoms.
Myth 2: CFS Can be Cured by Getting More Sleep
There is currently no causal or at least reliably effective treatment for CFS. Getting more sleep or resting do not reduce symptoms, especially as CFS patients do not generally consider their sleep to be restful.
The main problem is that we have not yet been able to identify clear causes for the etiology of CFS, which we might use to develop targeted treatments. Since, in the majority of cases, CFS is preceded by an infection (e.g. SARS‑CoV‑2 or the Epstein-Barr virus),13 experts are considering whether an infection might trigger permanent changes in the immune system and gut microbiome, which in turn might affect the brain by causing a reduction in neurotransmitters. The idea is that this may ultimately lead to, among other things, disorders of the autonomic nervous system – the part of the nervous system responsible for involuntary processes in the body, such as breathing, heartbeat, and metabolism – and to a reduction in cardiovascular performance.14 This is just one of many hypotheses; more recent etiological research focuses on the role of autoantibodies and mitochondria in particular.
As long as the cause of CFS has not been sufficiently identified, it can only be treated symptomatically, without being able to reach a cure. Since only supportive accompanying measures are available so far, studies suggest that less than 10% of those affected (mainly young adults before the age of 40, with women being around two to three times more likely to be affected by CFS than men)15,16 fully recover from CFS.17
The German Institute for Quality and Efficiency in Healthcare (IQWiG) was unable to identify any evidence of efficacy for a specific drug therapy in its status report dated 17 April 2023.18 Psychotherapeutic treatments could be categorised as useful only as a supplement – specifically to support coping with the disorder, but not to eliminate the underlying symptoms.19 Immunoadsorption, oxygen therapy and antibody therapy (e.g. ocrelizumab, inebilizumab) approaches are reported as being very promising.20
Based on current knowledge, interdisciplinary care should be recommended, with GPs playing a central role as points of contact, effectively acting as navigators for referrals to specialists for further diagnostics and treatment. Ultimately, the supportive treatments must be adapted to the individual’s particular symptoms, where “pacing” is the focus of attention. Pacing means energy management, so that patients remain within their own limits of functional capability, in order to avoid a crash and PEM.
Unlike in traditional rehabilitation programmes, for example, the aim of pacing is not to increase activity, but to remain within one’s physical limits.21 Based on this, additional measures can be trialled, which are focused on the specific symptoms of the patients. For example, individually tailored occupational therapy or neurocognitive training can be considered if a person suffers from cognitive impairments, and supportive cognitive behavioral therapy can be considered in the case of psychological complaints.
Another problem with treatment is that the disease often becomes chronic before CFS is even diagnosed. International studies suggest that up to 90% of people suffering the symptoms are undiagnosed or misdiagnosed22 and that it often takes many years of misdiagnosis and countless medical consultations with various specialists before the diagnosis of CFS is correctly made.23 It should not be forgotten that the diagnosis of CFS is still highly controversial in society and that practitioners sometimes don’t know enough about the clinical picture.24 In the worst case, this can lead to the initiation of measures which, instead of improving the condition, can worsen the symptoms if the patient’s limits are exceeded.
Conclusion
CFS cannot be cured by sleep, nor is there any causal therapy that has been discovered to date. The only support measures that can be offered to patients are symptom-orientated and are based on managing symptoms, taking into account the individual’s exertion limits. The existing medical care infrastructure is insufficient but there is hope for a causal therapy in the coming years.
Myth 3: CFS Patients Are Always Unable to Work
This myth does not apply across the board, as the question of occupational disability depends on the individual job profile in qualitative and quantitative terms, as well as the severity of the clinical picture and how much the person is restricted because of this.
Firstly, CFS sufferers can be assumed to have a strong tendency to become chronic, i.e. the symptoms do not improve within the six-month period relevant for the benefit assessment25 The clinical manifestation of CFS varies from individual to individual and can range from mild restrictions to being bedridden. It is estimated that around 25% of CFS patients are no longer able to leave their home or bed.26 More than 60% of CFS patients are unable to work, with the prognosis being extremely unfavourable, especially for those on sick leave for more than two to three years.27
This means that when assessing disability claims, it is important to determine not only whether CFS is present, but also to assess the severity. The freely accessible Bell disability scale, for example, a useful tool for categorising severity, as it can be used as the basis for a more detailed assessment of functional limitations and goes up in steps of 10 from 0 to 100. A score of 100 represents the absence of any symptoms, while a score of 0 corresponds to the highest level of severity, in which a patient is bedridden and in need of care.28
Regardless of a specific score, the Bell disability scale is a good reminder that non-medical aspects should be considered alongside medical ones. To assess the occupational capability, it is important to clarify what the specific requirements of the individual’s job were and to what extent the insured person worked in it. It certainly makes a difference whether an insured person works full-time or part-time, whether their role demands them to be physically active, whether they work from home and can organise their breaks, whether they are occupied in “quiet” desk work or have a stressful job with customer contact, or if they have management responsibility.
The assessment of the severity of functional limitations must not be based solely on the insured person’s subjective report. Rather, the key term here, similar to the process of evaluating mental health conditions in claims, is “plausibility check”, so that the insured person’s subjective account must be compared with external criteria.
Concerning myth 1, we have already listed diagnostic tools that can be used to check plausibility. If, for example, the insured person reports exertion intolerance and muscular fatigue, the question must be asked whether this can also be detected in a handgrip strength test. An IME must again contextualise the result in the context of other factors, e.g. the subject’s musculature and behavioral observations outside the examination situation.
It is essential for a plausibility check to enquire about a person’s daily routine to assess whether the restrictions claimed for the occupation also manifest themselves in their everyday life (as would be expected). If a person reports that they are bedridden, then their entire living and care situation should be checked. This starts with food shopping and ends with considering whether aids such as wheelchairs or walking aids are used and whether a level of care has been determined (if not, why not?).
An internet search on the person should be carried out to the extent legally possible. An analysis of the professional income development (including any additional earnings) before and after the beginning of the disorder and its relation to the insured benefits is also important. Another important piece of the puzzle for the plausibility check is whether the severity of the complaint matches the intensity of therapeutic measures. For example, if an insured person is willing to undergo a “medical marathon” of doctors’ appointments, including self-pay services, this indicates pronounced suffering and supports the subjective claim.
If you want to find out more about the plausibility check of primarily subjective complaints, it is worth taking a look at the freely accessible AWMF guideline 051‑029.29
Once fatigue and cognitive impairment are complained of, a comprehensive (i.e. more than two hours) neurological-psychiatric assessment as well as psychological testing can sometimes be useful. Deficits in alertness are frequently observed here, less so in the areas of memory or executive functions. Since the quality of IMEs depends strongly on knowledge of the clinical picture of CFS and the necessary components of a plausibility check, the expert should be asked about experience in this field before commissioning an IME.30 Overall, we recommend a cautious approach when commissioning IMEs for CFS.
Although the number of CFS patients is likely to have increased as a result of the COVID‑19 pandemic – some studies estimate a doubling of the number of cases compared to the pre-pandemic period,31 – we are not expecting a “wave” of CFS related disability claims. In this regard, even if the estimated initial figure of approximately 70,000 to 220,000 affected persons in the German adult population32 were doubled, the number of cases would still be comparatively low. This figure would have to be adjusted again according to the severity of the CFS, and selective effects with regard to the population of those people who take out occupational disability insurance would also have to be taken into account in a pre-selection by underwriting.
Conclusion
Without comprehensively clarifying the facts, it is not possible to draw the general conclusion that CFS automatically indicates occupational disability. In particular, considering the severity of a person’s CFS and a plausibility check are key. As a result, a massive increase in disability claims due to CFS is not expected in the coming years.
- Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin. (2024). AWMF‑S3-Leitlinie 053‑002 „Müdigkeit“ (p. 19 et seq.). https://register.awmf.org/de/leitlinien/detail/053-002 (last accessed on 31.10.2024).
- Hoffmann et al. (2024). Interdisziplinäres, kollaboratives D‑A‑CH Konsensus-Statement zur Diagnostik und Behandlung von Myalgischer Enzephalomyelitis/Chronischem Fatigue-Syndrom. Wien Klin Wochenschr 136 (Suppl 5), 103‑123 (2024). https://link.springer.com/article/10.1007/s00508-024-02372-y#citeas (last accessed on 31.10.2024).
- Ludwig et al. (2023). Myalgische Enzephalomyelitis/chronisches Fatigue-Syndrom: Eine Übersicht zur aktuellen Evidenz. Der Nervenarzt, 94 (8), 725‑733. https://pmc.ncbi.nlm.nih.gov/articles/PMC9875188/pdf/115_2022 _Article_1431.pdf (last accessed on 31.10.2024).
- Dreßing, H., & Dreßing, A. (2024). Forensisch-psychiatrische Implikationen bei Post‑/Long-COVID. Forensische Psychiatrie, Psychologie, Kriminologie, 18 (1), 71‑78. https://www.springermedizin.de/post-covid/begutachtung/forensisch-psychiatrische-implikationen-bei-post-long-covid/26541976 (last accessed on 31.10.2024).
- Kanadische Konsenskriterien für die Diagnose CFS/ME (Source: Charité, Berlin): https://cfc.charite.de/fileadmin/user_upload/microsites/kompetenzzentren/cfc/ZZ_alte_Dateien/Landing_Page/Kanadische_Kriterien_mitAuswertung.pdf (last accessed on 31.10.2024).
- Cotler et al. (2018). A brief questionnaire to assess post-exertional malaise. Diagnostics, 8 (3), 66. https://pmc.ncbi.nlm.nih.gov/articles/PMC6165517/pdf/diagnostics-08-00066.pdf (last accessed on 31.10.2024).
- See hand dynamometer test (Source: Charité, Berlin): https://cfc.charite.de/fileadmin/user_upload/microsites/kompetenzzentren/cfc/ZZ_alte_Dateien/Landing_Page/Hand_Dynamometer_Test.pdf (last accessed on 31.10.2024).
- Bateman et al. (2021). Myalgic encephalomyelitis/chronic fatigue syndrome: essentials of diagnosis and management. Mayo clinic proceedings, 96 (11), 2861-2878. https://www.mayoclinicproceedings.org/action/showPdf?pii=S0025-6196%2821%2900513-9 (last accessed on 31.10.2024).
- Renz‑Polster, H., & Scheibenbogen, C. (2022). Post-COVID-Syndrom mit Fatigue und Belastungsintoleranz: Myalgische Enzephalomyelitis bzw. Chronisches Fatigue-Syndrom. Innere Medizin, 63 (8), 830-839. https://pmc.ncbi.nlm.nih.gov/articles/PMC9281337/pdf/108_2022_Article_1369.pdf (last accessed on 31.10.2024).
- See endnote 2.
- Nacul et al. (2021). European Network on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (EURO-MENE): Expert Consensus on the Diagnosis, Service Provision, and Care of People with ME/CFS in Europe. Medicina, 57 (5), 510. https://pmc.ncbi.nlm.nih.gov/articles/PMC8161074/pdf/medicina-57-00510.pdf (last accessed on 31.10.2024).
- See endnote 9.
- See endnote 8.
- Walitt et al. (2024). Deep phenotyping of post-infectious myalgic encephalomyelitis/chronic fatigue syndrome. Nature Communications. https://doi.org/10.1038/s41467-024-45107-3; Eastman, P. (2024). NIH study provides long-awaited insight into myalgic encephalomyelitis/chronic fatigue syndrome. JAMA. https://pmc.ncbi.nlm.nih.gov/articles/PMC10881493/pdf/41467_2024_Article_45107.pdf (last accessed on 31.10.2024).
- Lim et al. (2020)., Systematic review and meta-analysis of the prevalence of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). J Transl Med, 18 (1), 100. https://pmc.ncbi.nlm.nih.gov/articles/PMC7038594/pdf/12967_2020_Article_2269.pdf (last accessed on 31.10.2024).
- Angelsen, A. & Schei, T. (2024). EMEA survey of ME/CFS patients in Europe: Same disease, different approaches and experiences. European ME Alliance (EMEA).
- Ghali et al. (2022). Factors influencing the prognosis of patients with myalgic encephalomyelitis/chronic fatigue syndrome. Diagnostics, 12 (10), 2540. https://pmc.ncbi.nlm.nih.gov/articles/PMC9600584/pdf/diagnostics-12-02540.pdf (last accessed on 31.10.2024).
- Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWIG). (2023). Myalgische Enzephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) – Aktueller Kenntnisstand. Final report from 17.04.2023. https://www.iqwig.de/download/n21-01_me-cfs-aktueller-kenntnisstand_abschlussbericht_v1-0.pdf (last accessed on 31.10.2024).
- Grande et al. (2023). The role of psychotherapy in the care of patients with myalgic encephalomyelitis/chronic fatigue syndrome. Medicina, 59 (4), 719. https://pmc.ncbi.nlm.nih.gov/articles/PMC10145115/pdf/medicina-59-00719.pdf (last accessed on 31.10.2024).
- See the interview with Prof. Dr. med. Carmen Scheibenbogen „Das erste zugelassene Medikament wird den Durchbruch bringen“ in „Der Spiegel“, edition 48/2024.
- See endnote 2.
- Solomon, L., & Reeves, W. C. (2004). Factors Influencing the Diagnosis of Chronic Fatigue Syndrome. Archives of Internal Medicine, 164 (20), 2241‑5.
- Habermann-Horstmeier, L., & Horstmeier, L. M. (2023). Die ärztliche Wahrnehmung von ME/CFS-Erkrankten (myalgische Enzephalomyelitis/chronisches Fatigue-Syndrom) als „schwierige Patienten“. Prävention und Gesundheitsförderung. https://www.researchgate.net/publication/373491694_Die_arztliche_Wahrnehmung_von_MECFS-Erkrankten_myalgische_Enzephalomyelitischronisches_Fatigue-Syndrom_als_schwierige_Patienten/link/64ef10f367890027e16db103/download (last accessed on 31.10.2024).
- See endnote 22.
- Legler et al. (2023). Long-term symptom severity and clinical biomarkers in post-COVID‑19/chronic fatigue syndrome: results from a prospective observational cohort. EClinicalMedicine, 63, 102146. https://pmc.ncbi.nlm.nih.gov/articles/PMC10469383/pdf/main.pdf (last accessed on 31.10.2024).
- Montoya et al. (2021). Caring for the Patient with severe or very severe myalgic encephalomyelitis/chronic fatigue syndrome. Healthcare (Basel), 9 (10), 1291. https://pmc.ncbi.nlm.nih.gov/articles/PMC8544443/pdf/healthcare-09-01331.pdf (last accessed on 31.10.2024).
- Bateman et al. (2015). Chronic fatigue syndrome and co‑morbid and consequent conditions: evidence from a multi-site clinical epidemiology study. Fatigue: Biomedicine, Health & Behavior, 3 (1), 1‑15; Vink, M., & Vink‑Niese, F. (2019). Work rehabilitation and medical retirement for myalgic encephalomyelitis/chronic fatigue syndrome patients. A review and appraisal of diagnostic strategies. Diagnostics, 9 (4), 124. https://pmc.ncbi.nlm.nih.gov/articles/PMC6963831/pdf/diagnostics-09-00124.pdf (last accessed on 31.10.2024).; Adamowicz et al. (2014). Defining recovery in chronic fatigue syndrome: a critical review. Quality of Life Research, 23 (9), 2407‑2416.
- Bell, D. S. (1995). The doctor’s guide to chronic fatigue syndrome: Understanding, Treating and Living with CFIDS. Boston: Da Capo Lifelong Books.; see also Charité, Berlin: https://cfc.charite.de/fileadmin/user_upload/microsites/kompetenzzentren/cfc/ZZ_alte_Dateien/Landing_Page/Kanadische_Kriterien_mitAuswertung.pdf (last accessed on 31.10.2024).
- AWMF‑S2 k‑Leitlinie 051‑029 „Begutachtung psychischer und psychosomatischer Störungen“. https://register.awmf.org/de/leitlinien/detail/051-029 (last accessed on 31.10.2024).
- See endnote 4.
- See endnote 9.
- See endnote 17.





