-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Structured Settlements – What They Are and Why They Matter
Publication
PFAS Awareness and Concern Continues to Grow. Will the Litigation it Generates Do Likewise?
Publication
“Weather” or Not to Use a Forensic Meteorologist in the Claims Process – It’s Not as Expensive as You Think
Publication
Phthalates – Why Now and Should We Be Worried?
Publication
The Hidden Costs of Convenience – The Impact of Food Delivery Apps on Auto Accidents
Publication
That’s a Robotaxi in Your Rear-View Mirror – What Does This Mean for Insurers? -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Key Takeaways From Our U.S. Claims Fraud Survey
Publication
Favorite Findings – Behavioral Economics and Insurance
Publication
Individual Life Accelerated Underwriting – Highlights of 2024 U.S. Survey
Publication
Can a Low-Price Strategy be Successful in Today’s Competitive Medicare Supplement Market? U.S. Industry Events
U.S. Industry Events
Publication
The Latest in Obstructive Sleep Apnea -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
The Impact of Diabetes on Latin America

May 14, 2019
Saskya Córdova
Region: Latin America
English
Español
According to the World Health Organization, diabetes is the second-most common cause of death in Mexico and one of the top 10 causes of death globally.1 It is a non-communicable disease, wherein the plasma glucose levels increase over the regular limit for a healthy person. Some risk factors for diabetes include lifestyle, genetics, obesity, age and gender.
From 1990 until 2014, the global number of cases of people with diabetes quadrupled to 422 million. Even though people may know that diabetes can cause severe complications in their health as well as increase their risk of premature death, not everyone prone to developing diabetes follows appropriate treatment. During the past decade in Latin America, the growth of a middle-class population engendered the rise of sedentary lifestyles and unhealthy diets, which have increased the incidence of risk factors for diabetes. This, combined with the lack of prevention and access to proper healthcare, has generated a higher prevalence rate and mortality risk. However, an adequate and affordable insurance solution could help raise awareness and provide economic support in the situation of a diabetes-related event that may entail significant costs.
In Mexico a national health survey called ENSANUT (Encuesta Nacional de Salud y Nutrición) is conducted every six years. Using information from the health survey, this article presents a Generalized Linear Model (GLM) analysis of different variables that are correlated to diabetes in the Mexican population and could be helpful for the analysis of other Latin American countries. The analysis focuses on risk factors for diabetes, such as gender, age and socio-economic status. Moreover, since environmental risk factors – such as high body mass index (BMI) – can produce early complications of the disease, including deaths, we present an analysis of the percentage of deaths due to this risk. Finally, we discuss the health costs of diabetes in Latin America and the challenges that the insurance industry is facing.
Types of diabetes: What are the differences?
There are two main types of diabetes. Type 1 diabetes is an autoimmune disease caused by an insulin insufficiency that is often diagnosed in childhood and is not associated with an excess of body weight. On the other hand, type 2 diabetes is often associated with overweight, old age and family history. It is the most common type of diabetes worldwide and usually diagnosed in adults above 30 years old. While current medical knowledge cannot prevent type 1 diabetes, there are effective approaches to prevent type 2 diabetes, its complications and possible premature death.2
Incidence rates of diabetes in Latin America
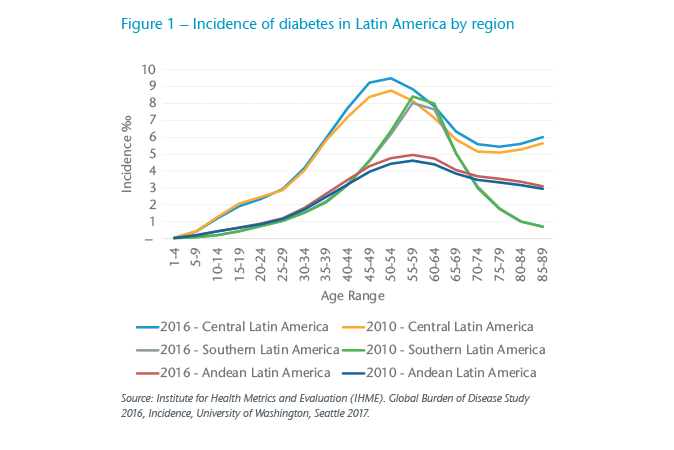
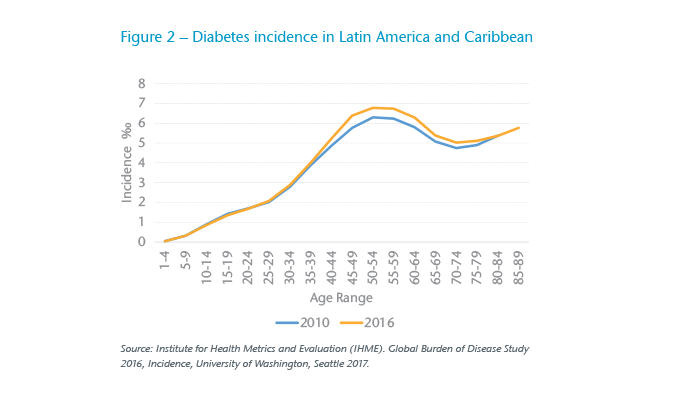
Diabetes prevalence and incidence rates have been increasing faster in low and middle-income countries, as is the case in Latin America.3 Based on information from the 2016 Global Burden of Disease Study, the incidence rate of the region increased from 2.74‰ in 2010 to 3.06‰ of all cases in 2016. For this analysis, Latin America was divided into three regions as seen in Figure 1: Central Latin America (Mexico, Panama, Colombia, Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, Venezuela), Andean Latin America (Bolivia, Ecuador, Peru) and Southern Latin America (Argentina, Chile, Uruguay). Figure 1 shows that the incidence of diabetes in Central Latin America is 2.17 times higher than the Andean Latin America Region and 1.71 times higher than Southern Latin America. The higher incidence in Central Latin America can be a consequence of the statistical impact that Mexico has in this region where diabetes is considered the major health problem of the country. Moreover, in Central Latin America the fast food influence is higher than in other regions of Latin America, generating diet-related health problems and therefore an increase in the incidence of diabetes. Despite the different pattern of incidence growth in each region shown in Figure 1, Figure 2 shows a positive correlation between the rise of diabetes incidence and age increase in the whole region of Latin America and Caribbean. However, it is interesting to note in both Figure 1 and 2 that after the age of 65 the incidence rates start to fall. This decrease can be explained by the fact that people are diagnosed at early ages instead of older ages, resulting in a reduction of the incidence considerably in the older population.
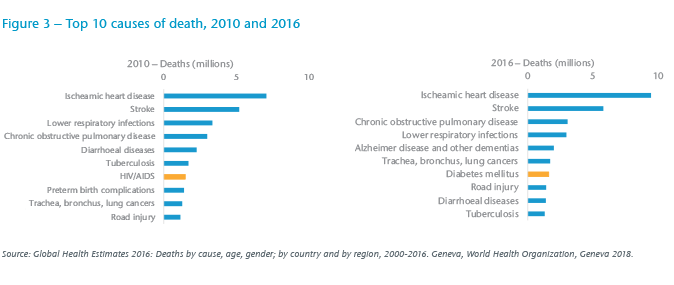
In addition to the increasing incidence of diabetes, the risk of death from diabetes also increased. Deaths due to diabetes represented 10.7% of the global all-cause mortality and were one of the top seven causes of death in 2016 – higher than deaths caused by infectious diseases, such as HIV/AIDS (Figure 3). Of all the regions in the world, according to the International Diabetes Federation (IDF) report, South and Central America are the only regions presenting an increased mortality trend, which underscores the importance of analyzing the risk factors influencing the disease.4
Risk factors for diabetes
Prevalence of diabetes by sociodemographic factors – GLM (Generalized Linear Model)
The increasing number and complications of type 2 diabetes cases can be linked to sociodemographic factors and environmental risks. As projected by the IDF, the prevalence rate of diabetes in South and Central America is expected to rise by 62%, increasing from 26 million cases in 2017 to 42 million in 2045. In Mexico the estimated 12 million cases in 2017 are expected to rise by 35% to an estimated 16 million cases by 2045.5
Using the information from the 2016 ENSANUT survey, we examined the effects of the sociodemographic factors on diabetes in Mexico. The prevalence was modeled by a GLM that allows us to see the relationship of independent variables (e.g. age or gender) with a dependent variable, in this case the presence of diabetes.
We chose a Poisson distribution to model the number of diabetes cases, and we modeled the impact of four demographic factors on the prevalence of diabetes.
All of the analyzed variables proved to be statistically significant (p-value below 5%):
- Gender
- Age
- Level of Education
- Socioeconomic Status
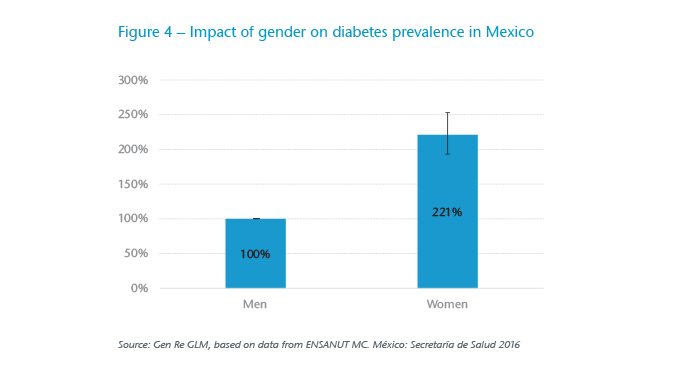
Impact of gender
The analysis shows a strong correlation between gender and the prevalence of diabetes (see Figure 4): women have twice the risk of developing diabetes than men. This trend might be explained by the new era of globalization and modernization in Mexico, where females are increasingly joining the workforce. Lifestyles are changing from an era of cooking fresh food at home to the easy access and consumption of processed food in all price ranges. Moreover, there is a higher prevalence of obesity in females in Mexico, a factor that can be strongly correlated to the higher cases of diabetes.
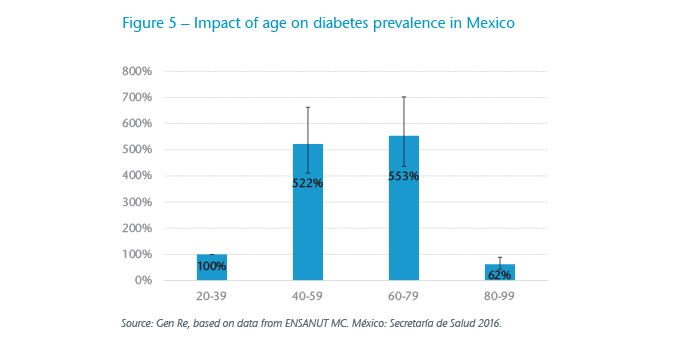
Impact of age
In our GLM, we analyzed the impact of diabetes by four age groups:
- Group 1: 20-39
- Group 2: 40-59
- Group 3: 60-79
- Group 4: 80-99
The results show that when holding all other risk factors constant, the likelihood of diabetes in adults between age 40 to 79 is five times higher than the likelihood of diabetes in adults between 20 to 39 years old (Figure 5). This may be explained by the loss of the body’s ability to metabolize sugar as it increases in age. In addition, genetics and unhealthy diets in early ages also have a direct impact on the increase of diabetes cases at older ages. In the analysis, we found that people between age 80 and 99 years old have lower prevalence of the disease than adults between 20 to 39 years old, most probably caused by a bias in the survey where people may have died before being interviewed, therefore preventing the influence from being observed.
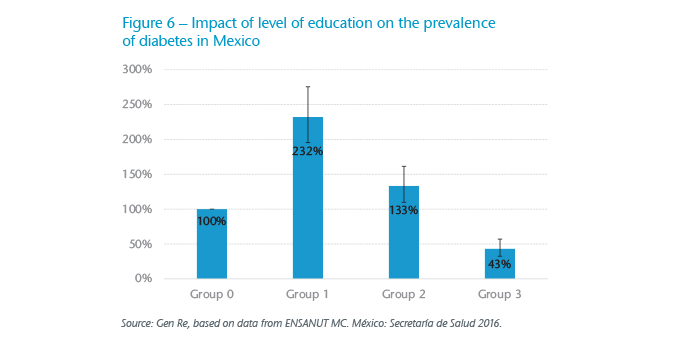
Impact of Level of Education
For this analysis, we divided education into four groups:
- Group 0: Adults with no primary education
- Group 1: Adults with primary education
- Group 2: Adults with high school education
- Group 3: Adults with university degree, Master’s and PhD
Results showed that people with basic education level in Mexico have a higher likelihood of being diabetic than those who have achieved a university degree. People with a university degree have 43% the risk of developing diabetes compared to those with no primary education (Figure 6). Moreover, it is interesting to notice the difference between people with no primary education and those individuals with only a primary education. People in Group 1 and Group 2 present a higher risk of diabetes than the ones in Group 0. This may be explained by the fact that individuals with no primary education may be less influenced by modern lifestyles and processed products, which are easily available in bigger cities where education is available.
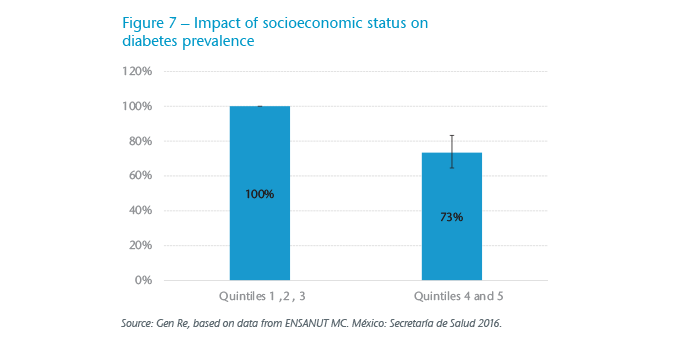
Impact of socioeconomic status
Finally, we concluded the GLM analysis by examining the effect of the socioeconomic status. For that purpose, we used the information from ENSANUT and evaluated the effect on quintiles.6 Quintile 1 represents the segment of the population with the lowest income and quintile 5 represents those with the highest income level.
For the analysis, we divided quintiles into two levels:
- Level 1 (Low and Middle Income): Quintiles 1, 2 and 3
- Level 2 (High Income): Quintiles 4 and 5
As shown in Figure 7, we can conclude that people with a Level 1 income have a higher risk of diabetes and therefore present a higher number of cases. This result is in line with what we found in the previous analysis. The higher number of diabetes cases in the low- and middle-income groups can be influenced by the lack of health promotion and prevention campaigns.
Environmental risks
We observed in Latin America an increase of sedentary lifestyles accompanying the rise of the middle class. Diets full of carbohydrates and limited physical exercises are strongly affecting the way people develop diabetes complications.
Overweight and obesity have become major health problems in many parts of the world. In 2016 the World Health Organization (WHO) reported that 39% of adults (>18 years old) were overweight and 13% were obese. Mexico was ranked as one of the top ten countries with a high prevalence of obesity.
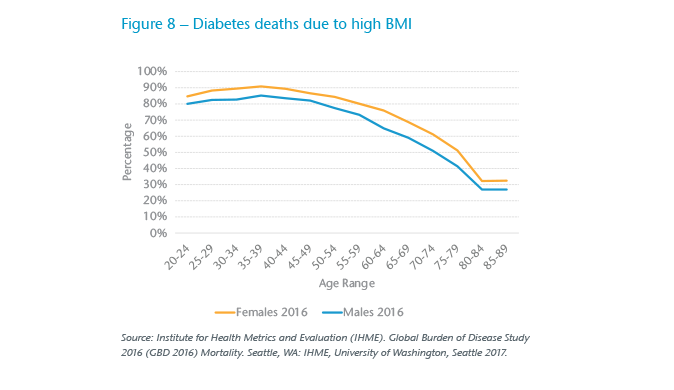
In order to analyze the percentage of deaths caused by diabetes type 2 in Mexico due to the high BMI risk factor, we used information from the 2016 GBD. BMI is the most frequently used measure to evaluate the proportion of body fat of an individual, as it analyzes an individual’s weight in relation to his/her height. Based on the WHO classification, adults with a BMI higher or equal to 25 are considered as overweight and those with a BMI greater or equal to 30 as obese (OECD, 2017). There is a relation between high BMI (overweight and obesity) and diabetes deaths. As shown in Figure 8, diabetes deaths related to a high BMI are greater for adults between 25 to 45 years old. The influence of high BMI on diabetic deaths start to decrease after the age of 60, this might be caused by the fact that BMI starts to play a less important role and other factors – such as blood pressure and high cholesterol – outweigh the effect of a high BMI. In addition, at higher ages it can get harder to precisely define that diabetes deaths were caused due to a low or high BMI.
Environmental risks are similar in importance to demographic factors and have to be considered when developing an insurance product. Factors, such as BMI, are already used when underwriting diabetes risks. In addition, glycosylated hemoglobin (HbA1c), which measures the average level of glucose or blood sugar of an individual during the previous three months, has become an important marker to design diabetes insurance solutions.7 Studies have proven a strong association between high glycemic levels and the increasing risk of all-cause mortality for females and males.8 Results of a research study conducted in Mexico City showed the increase in mortality due to the worsening glycemic control on a cohort of 100,000 women and 50,000 men.9 The results indicated a rate of 5.2 deaths for participants with HbA1c less than 9%, and 10.5 deaths for those with HbA1c of 11% or higher. Consequently, the number of deaths doubled with an increase of two percentage points on the HbA1c level. This finding indicates the need to improve diabetes management and reduce the premature mortality by increasing glycemic control and early diagnosis.
Diabetes insurance – Its role in reducing the economic burden of diabetes and its challenges
Health costs in Latin America
Independent of the income levels of different countries, diabetes represents a high economic cost for all regions and therefore an increase in the economic burden as well. In Latin America, the increased amount of healthcare expenditure dedicated to diabetes treatment and related complications shows the opportunity that exists for insurance companies to provide sustainable products with a dual value proposition: (a) provide economic support to those that require high amounts of money for diabetes management and (b) become profitable at the same time.
The IDF reported that healthcare expenditure on diabetes has increased tremendously, having a great impact on healthcare budgets worldwide. The expenditure in South and Central America in 2017 represented USD29.3 billion (10.6% of the total healthcare budget of the entire region) and is expected to grow by 30% until 2045, reaching an approximate of USD38.1 billion. Mexico on its own is ranked number 8 on the top 10 countries with highest healthcare expenditure due to diabetes, which is expected to have reached USD19 billion in 2017.
Even though the goal of many countries in Latin America has been to develop a universal health insurance program, they are not focused on all phases of a disease but rather focused on the healing and rehabilitation phase, to the neglect of the prevention/diagnosis phases. With a well-implemented primary care system in terms of diagnosis/prevention and education about the illness, countries can reduce health costs emerging from complications caused by a lack of medical intervention at the right phase of the illness.10
The role of insurance and the challenges of pricing diabetic products
Health insurance can benefit societies by improving awareness about diabetes. Nowadays products are usually designed for two population segments: healthy people and people with diagnosed diabetes. The products aim to provide economic relief for people who must cover expenses arising from diabetes.
In general, the products offer increased awareness of the disease by providing extra benefits due to correct health management. For this purpose, insurance companies have started to build partnerships with InsurTech providers to offer wellness features, such as online platforms or applications to track medical values or provide health coaches with diets and fitness plans. These measures can provide a satisfactory experience and an effective management of the disease that could prevent complications or premature deaths.
However, as analyzed previously, the risk of diabetes can be directly affected by sociodemographic and environmental risks, which makes the pricing of diabetes insurance a very challenging task.
Depending on the product, the pricing may vary considerably. Risk premiums for diabetic lives are mainly determined by HbA1c level and age. Nonetheless, other factors – such as blood pressure, cholesterol level and duration of the disease – also have an impact. Then another challenge arises from the high number of associated risk factors that must be analyzed to get the best estimate rate.
When underwriting diabetes, the high risks involved in the disease require information, such as BMI, cholesterol, blood pressure and family history. This high dependency on identifying risk factors makes the underwriting processes long and unattractive to potential clients. The challenge faced by the insurance industry is to develop a more appealing underwriting process. At the same time, the industry needs to implement processes to monitor the HbA1C levels of the insured on an ongoing basis, as these levels can get worse over time.
Conclusion
The insurance industry can help to raise awareness and provide economic support for a diabetes-related event, which implies high costs. However, designing products for diabetic risks becomes complicated due to the number of risk factors that influence it. Our GLM confirmed the existence of a strong correlation between certain sociodemographic factors, such as age, gender, socioeconomic status and the prevalence of diabetes. Women seem to face a higher risk of getting diabetes than men, and with age the probability of developing diabetes increases. Therefore, we see the importance of diabetes products being founded on a risk premium basis that allows us to reflect the real risk related to an individual’s diabetes disease. Besides sociodemographic factors, measurements – including HbA1c, blood pressure, cholesterol and BMI – are required to differentiate the rates and design the insurance product. Good monitoring of health factors, such as HbA1c, may help us to control the real glycaemia of the insured, prevent future complications and improve the insurance benefits.
A big question the insurance industry faces in Latin America is how we can approach diabetics risks and offer them an insurance solution that considers:
- An attractive product with valuable features, which can meet the needs of the population; and
- Pricing the product according to all related risks.
In Latin America, low and middle-income people do not have access to these products due to the low number of product offerings with diabetic insurance solutions and the high costs associated to them. We are eager to learn from the experience of other more developed markets and use available data that can help us to create new attractive solutions for a society that needs protection if a chronic disease, such as diabetes, affects their lives.




