-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Structured Settlements – What They Are and Why They Matter
Publication
PFAS Awareness and Concern Continues to Grow. Will the Litigation it Generates Do Likewise?
Publication
“Weather” or Not to Use a Forensic Meteorologist in the Claims Process – It’s Not as Expensive as You Think
Publication
Phthalates – Why Now and Should We Be Worried?
Publication
The Hidden Costs of Convenience – The Impact of Food Delivery Apps on Auto Accidents
Publication
That’s a Robotaxi in Your Rear-View Mirror – What Does This Mean for Insurers? -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Key Takeaways From Our U.S. Claims Fraud Survey
Publication
Favorite Findings – Behavioral Economics and Insurance
Publication
Individual Life Accelerated Underwriting – Highlights of 2024 U.S. Survey
Publication
Can a Low-Price Strategy be Successful in Today’s Competitive Medicare Supplement Market? U.S. Industry Events
U.S. Industry Events
Publication
The Latest in Obstructive Sleep Apnea -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Why Insurers Should Give Weight to the Global Rise in Eating Disorders

April 27, 2017
Dr. Chris Ball
English
The magnitude of the cost, both to the individual and the economy as a whole, represented by eating disorders is often underestimated. The growing numbers presenting to services in high income countries is not merely a reflection of service availability, but a very real increase in the number of cases.
In the EU alone, an estimated 20 million people have an eating disorder with an economic impact amounting to one trillion euros a year. The financial costs are similar to those of anxiety and depression, whilst the “burden of illness” costs are even higher. One in every six/seven young women has an eating disorder (anorexia nervosa (AN); bulimia nervosa (BN); binge eating disorder (BED); and related syndromes), making it at least as common as type 1 diabetes. Life-time prevalence estimates are consistently higher for BED (1.4 %) than BN (0.8 %). One in every two/three people with BN or BED is obese, or will become so, rendering them at risk of developing related complications.1
For many years it was assumed that eating disorders were the preserve of rich Western societies where food is abundant and relatively cheap. Over recent years it is increasingly recognised that these disorders also present in other societies but the diagnostic criteria usually employed may fail to identify those who experience the diseases in these cultures.2
Although the peak age of onset is between 15 and 25, a time of significant development in biological, psychological and social terms, the illness is presenting in younger and younger children. The often-applied stereotype that only women develop eating disorders is almost, but not quite, true for AN. A recent Dutch study recorded only 0.1 % of adolescent males with the illness compared to 1.2 % of females, but this is not the case for BN where the proportions are much more even.3
Broadly speaking, the average duration of an eating disorder is six years. Mortality rates are almost twice those of the general population, and for those experiencing AN the rates are nearly six times as great – much higher than the mortality of other disorders of young adulthood, such as asthma and type 1 diabetes. Those experiencing eating disorders will often find it difficult to sustain employment, suffer comorbid mental health and physical health problems and experience a low quality of life particularly when fighting a long-standing chronic illness. These disorders also take a significant toll on families. Relatives with eating disorders are reported to be a higher burden than relatives with depression or schizophrenia.4
Symptoms of eating disorders
The symptoms of the three commonest eating disorders described in American Psychiatric Association’s DSM-5 are compared in Table 1.
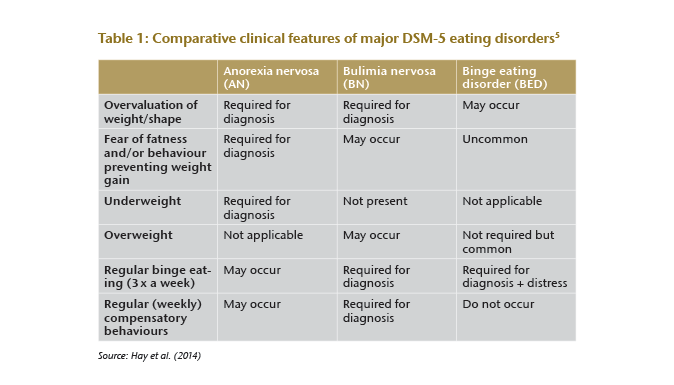
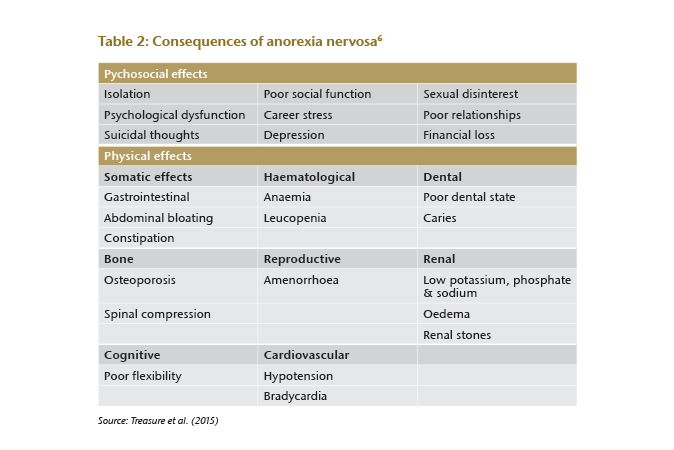
A diagnosis of AN requires behavioural disturbances that significantly restrict energy intake, leading to a significantly low body weight coupled with a disturbance in the individuals’ experience of their body shape and weight. The individual also harbours an intense fear of gaining weight. Those with “restricting type” AN lose weight primarily by fasting and exercise whilst the “binge eating/purging type” induces vomiting and may also use enemas, laxatives and diuretics to reduce their weight. Clearly these behaviours will have a profound effect on many systems of the body, bringing their own complications, essentially those of starvation (see Table 2).
Although patients with BN rely unduly on their perception of body weight when evaluating themselves, they are much less likely to be underweight than those with AN. A recurrent cycle of consuming large amounts of food followed by “compensatory behaviours”, similar to those of AN, is accompanied by a feeling of lack of control over eating.
By contrast BED is not accompanied by compensatory behaviours or an over-reliance on weight during self-evaluation. Lack of control of eating is present, as is distress at the amount one is eating, along with a sense of depression, disgust and guilt. BED occurs in individuals of normal to excess weight. In each of these disorders, a high likelihood exists for substantial problems in managing day-to-day roles in school, at work or as a parent, which may persist into later life.7
Comorbid disorders
Comorbid mental health problems are frequent; for AN this has been described as the “rule rather than the exception”. Anxiety and depression are both common; some experience obsessive compulsive symptoms, and the presence of a personality disorder is likely to lead to a worse outcome.8
People diagnosed with BED are highly likely to meet the criteria for other eating disorders at some point in their lives. They also experience other mental health problems, which include – in order of frequency – major depressive disorder, bipolar disorder, anxiety disorders, post-traumatic stress disorder and suicide attempts.9 BED is also associated with medical complications that are related to obesity. Prospective studies link the disorder to type 2 diabetes and metabolic syndrome as well as non-obesity-related disorders: asthma and gastrointestinal symptoms. Amongst women these may be menstrual dysfunction, pregnancy complications, intracranial hypertension and polycystic ovary syndrome.10
Mortality
A number of technical difficulties arise in interpreting the mortality studies for those who experience AN. Study populations vary, as do diagnostic criteria, length of follow-up and age structure, all of which can influence the outcomes. However, all studies agree that mortality of AN patients has significantly increased compared to the general population.
A meta-analysis of 35 studies reported a crude mortality ratio (CMR) of 5.1 deaths (95 % CI: 3.99 – 6.14) per 1000 person-years, i. e. 5.1 % per decade or 0.51 % per year for AN over a follow-up of 14 years. The longer the follow-up, the lower the mortality rate. Older age and low BMI at presentation, alcohol abuse, history of hospitalisation and suicidal behaviour are strong predictors of mortality. Suicide accounts for 20 % to 30 % of deaths (largely early in the course of the illness), the remaining mortality being caused by somatic complications.11
BN is less well studied but a meta-analysis of 12 studies described a mortality rate of 1.74 per 1000 person-years. The overall SMR was 1.93 (95 % CI: 1.44 – 2.59).12 Crow et al. (2009) examined mortality, in a sample of 906 BN patients at an out-patient clinic, between 1979 and 1997. A mean follow-up of almost 19 years found that 35 (3.9 %) had died, and suicide accounted for 23 % of deaths.13
Mortality in BED is much more difficult to define as it has been even less intensively studied and largely in those who have been hospitalised. The situation is complicated by the presence of obesity, which raises the risk of death in its own right.14 Suicide risk is possibly lower in this group than in other eating disorders.15
Management of eating disorders
Most developed countries have seen an increase in the numbers presenting for treatment over recent years.16 In the most severe forms of AN, inpatient treatment is indicated for refeeding, which must be undertaken with care to avoid “overfeeding syndrome”.17 The precise components of inpatient therapy are not well-described and most patients require follow-up outpatient work.
Many more are treated with a variety of psychological interventions as outpatients. Family-based interventions have been at the core of therapy over the years but, again, these are often not well-structured or defined. The Maudsley Model of Anorexia Treatment for Adults (MANTRA) targets specific domains central to the maintenance of AN for treatment: inflexibility and over-attention to detail, impairments in the emotion-social domain, positive beliefs about how AN helps the person and the unhelpful responses of families. This highly structured therapy has demonstrated positive results compared to other treatment.18 Pharmacological therapies have very limited use in managing core symptoms but may be valuable for treating comorbidities.
Cognitive behavioural approaches, including enhanced cognitive behavioural therapy (CBT) and CBT-guided self-help, are most useful for adults with BN and BED. Some evidence shows that other forms of therapy, interpersonal therapy (IPT) and dialectical behaviour therapy (DBT) may also help. Medication has a clearer impact with BN and BED patients than with AN, as both selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) have been associated with reductions in symptoms in both BN and BED.19 The stimulant drug lisdexamfetamine dimesylate (LDX) is the only drug approved by the FDA for the treatment of BED in adults. It is not clear if the outcome of bariatric surgery in this group is as good as in patients without BED. Particular care is needed during follow-up.20
Whilst this evidence base is vital in establishing appropriate treatments, the views of experienced clinical practitioners and patient perspectives also need to be taken into consideration if management is going to be successful.21
Eating disorders in males
The ratio of females to males for the different eating disorders has been referred to above. These figures may be skewed by under-reporting and under-detection in the male population. Among men, the lifetime prevalence of AN is 0.2 % to 0.3 %, of BN 0.1 % to 0.5 %, and of BED 1.1 % to 3.1 %, depending upon the population studied and criteria used. The changes to DSM classification should allow eating disorders in men to be more specifically diagnosed.22
The bodily concerns of males are rather different than those of females. The concern is not only about weight or thinness but also about muscularity. This leads to concerns about athleticism and hence excessive exercise rather than binge eating/purging symptom patterns. Men face a double stigma, not only that of experiencing a mental health disorder but one that is commonly thought to be experienced only by females. This leads to later recognition and a lack of gender-specific information and treatment. Paradoxically, the cultural stereotypes of eating disorders (EDs) mean that males with EDs are more newsworthy, so newspaper stories of men with EDs are increasingly common. Whilst this would normally reduce stigma, the sensationalism used to capture the reader’s attention may have tipped the balance back towards stigmatisation.23
If hospitalised with AN, men tend to be admitted at a slightly later age and for a shorter time than women. They most commonly report restriction of food intake and excess exercise rather than binging and purging. With severe AN, long-term survival does not appear to differ between the sexes but men died sooner after discharge from hospital, with the restrictive subtype having higher mortality.24 Across the spectrum of eating disorders, excess mortality has been reported for men compared to controls, but to a lesser degree than for women with comparable disorders.25
The future
For researchers the future task is to move from symptom-based categorical diagnosis towards a “neurobiologically grounded and dimensional classification of eating disorders”. For example, is AN a single condition or are there multiple “anorexias” with different causes, co-morbidities, brain changes and illness patterns? Not much is understood about the sequence or combinations of treatments to use if first-line interventions do not lead to recovery or improvement.26
New treatment modalities – from structured programs of psychological and behavioural intervention through to organic treatments that build on developing an understanding of the neurobiology of food and reward systems – promise an improvement in outcomes not seen for many years.27
Underwriting risk in eating disorders
The excess mortality exhibited by eating disorders, particularly AN, is of concern to underwriters. The outcome studies are often difficult to interpret in individual cases and care must be taken when applying these figures to the insured population. Those who apply for insurance are more likely to be in the good outcome group. Underwriters should be looking at the current BMI, length of illness, mental health comorbidities and suicide attempts as indicators of likely risk.
People who make good recoveries after short illnesses, maintain their weight, have good social adjustment and are without mental health comorbidities are unlikely to be at risk of significantly greater mortality than the population as a whole.





