-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Florida Property Tort Reforms – Evolving Conditions
Publication
Is Human Trafficking the Next Big Liability Exposure for Insurers?
Publication
When Likes Turn to Lawsuits – Social Media Addiction and the Insurance Fallout
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Understanding Physician Contracts When Underwriting Disability Insurance
Publication
Voice Analytics – Insurance Industry Applications [Webinar]
Publication
GLP-1 Receptor Agonists – From Evolution to Revolution U.S. Industry Events
U.S. Industry Events
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Thyroid Cancer and Critical Illness – Incidentally Speaking

March 05, 2015
Dr. (Celia) Ying Zhang,
Dr. Ian Cox
English
The thyroid is a physically insignificant endocrine gland located in the neck anterior to the trachea. Cancer of the thyroid has historically been uncommon, yet incidence rates have been increasing dramatically worldwide over the past 20 years. A corresponding increase in thyroid cancer claims has also been observed in Critical Illness (CI) insurance over the past decade.
The nation with the highest levels of incidence is the Republic of Korea, where it is now the most frequently reported cancer in women with an incidence double that of breast cancer. If a similar surge in incidence rates were to be repeated in other countries, it could pressurise CI pricing, leading to either a substantial increase in premium rates or the imposition of exclusions for early thyroid cancer in policy definitions.
The vast increase in the reported thyroid cancers has been due to one particular histological type called Papillary Thyroid Cancer (PTC); Medullary, Follicular and Anaplastic tumours of the thyroid have not increased in incidence. The size of these PTC tumours is predominately less than 2 centimetres (cm) in size with most below 1cm. Many specialists label these small tumours “microcarcinomas”, although some reserve this term for those below 0.5cm. It is of relevance to CI definitions that there is no stage 0, pre-invasive stage or carcinoma-in-situ in the accepted staging systems of thyroid cancer. This means that tissue is either described as “benign” or “malignant” with no pre-malignant category in the histological classification. This article looks at the possible causal factors of the increased incidence across the world, and the implications this may have for CI products.
Increasing incidence
Korea has the highest incidence rates of PTC and the fastest rate of increase of any country. In females, rates have increased by 20.7% year-on-year from 1999 to 2011. In 1999 the age-standardised incidence rate in Korean females was 11.9 per 100,000, but by 2011 this had risen to 113.8 (see Figure 1).
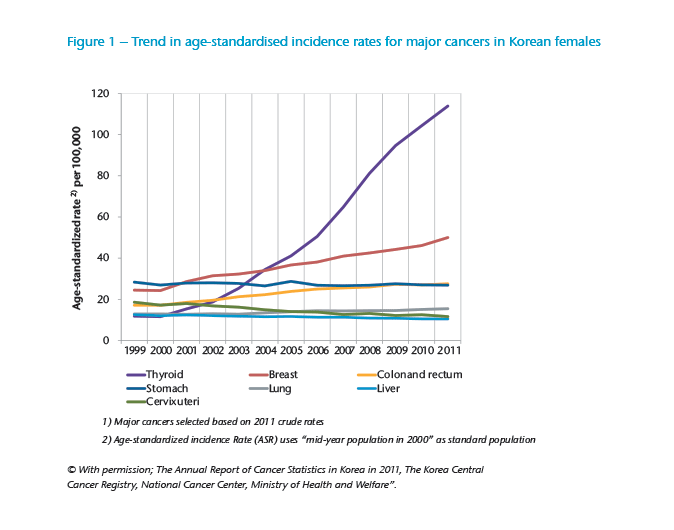
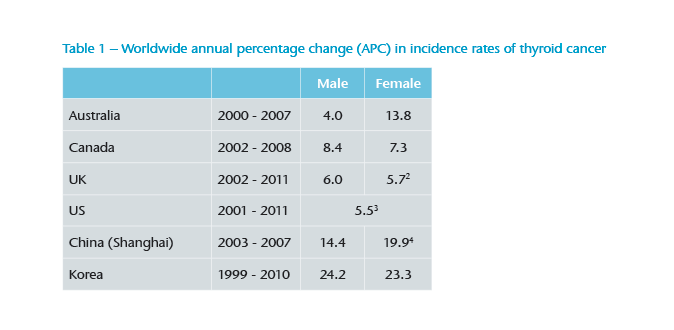
Other countries are experiencing a lower absolute incidence rate – commensurate with the rates seen in Korea during the 1990s – but the speed of the rise in incidence suggests that thyroid cancer will become a potentially serious issue for CI elsewhere (see Table 1).1
The age distribution for cancer of different sites in Korea is shown in Figure 2. Thyroid cancer incidence in males is strongly related to age, with the highest incidence rates being in older men. However, incidence in females is unusual as it does not follow the same pattern of increasing incidence with age seen in males (and most other cancers).
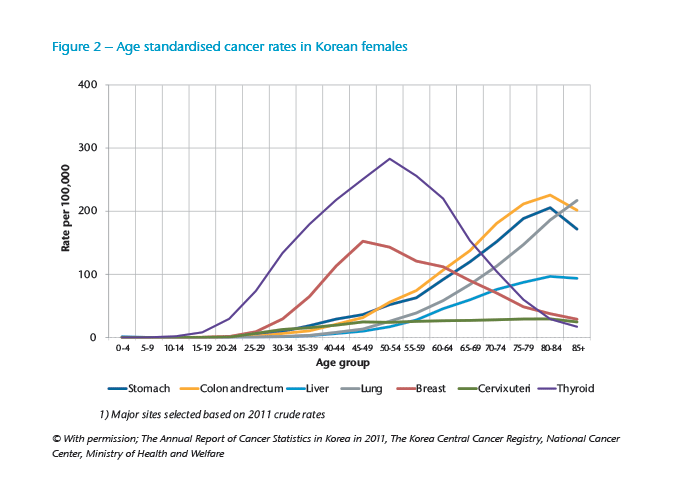
PTC mainly affects women, with a female-to-male ratio of 5:1 in Korea compared to 2.5:1 in the UK. The peak incidence occurs at a much younger age than is seen in many other cancers. This has significant implications for CI because the strong increase and the peak affect much younger ages and earlier durations.
Impact of screening
There is evidence that the rise in incidence of PTC in Korea results from “overdiagnosis” of small lesions that would not have become clinically significant in a person’s lifetime – borne out by the fact that mortality from thyroid cancer has not increased in spite of a massive increase in detection. There is a clear correlation between the amount of screening and the number of thyroid lesions found.5
In Korea screening for cancer is much more popular, and as a consequence it is detected more frequently. The Korea National Cancer Screening Program recommends regular screening only for stomach, breast, cervix uteri, liver and colorectal cancer. However, screening for thyroid cancer is opportunistic, relying on the selling of an ultrasound of the neck as an additional procedure to asymptomatic individuals while in a medical environment, and varies depending on the medical institution.
No country has an organised national screening programme to detect thyroid cancer. It seems unlikely that any country would do so given the very low mortality from thyroid cancer in spite of the increasing incidence. However, radiological imaging with CT or MRI scanning of the head or chest, which has increased significantly in recent years, often provides images of the neck incidentally. These may reveal thyroid lesions as an incidental finding. Once identified, it is difficult to avoid further investigation, including biopsy, even when the likelihood of subsequent health benefits is low. The disparity between rising incidence and flat mortality rates is one marker that supports the concept of overdiagnosis of thyroid cancer.
Underlying cause
While most observers accept that the increased incidence is driven by increased use of modern imaging technologies, others argue it is not the sole explanation. There is some evidence in the US that, even when people emigrate, those from Asian countries have higher rates of diagnosis than native populations, although the reported increase was in South Asians rather than those from North Asia, including China and Korea.6 Obesity has been implicated as a risk factor for thyroid cancer as it has for several malignancies. One large study showed a moderate but significant increase in risk with increasing BMI.7
Iodine is an integral component of thyroid hormones, so the metabolism of the gland is linked to the availability of iodine in the diet. In areas of iodine deficiency, goitres are common and there is a higher proportion of Follicular Thyroid tumours. Where there is adequate iodine, as when supplemental iodine is added to salt, the proportion of PTC rises. Increased exposure to radiation is one potential environmental contributing factor, and it has been shown that the exposure to radiation has increased mainly in the US population over the past 25 years mainly due to medical imaging technology. Events such as the Chernobyl disaster have shown that environmental radiation is a cause of thyroid cancer in those exposed at a young age.
Of all the possible drivers, the most important appears to be the access to high levels of medical care. There is a clear correlation between the access to and numbers of ultrasound scans performed and the incidence of diagnosed thyroid cancers.8 Again, the implication is that the increase is more related to overdiagnosis than a true increase in incidence. There is no evidence to suggest that the rates reported in Korea cannot be replicated elsewhere.
Thyroid and Critical Illness
If all thyroid cancer is included with the scope of CI coverage, an assessment of the maximum numbers of possible diagnoses is required if pricing is to reflect the risk adequately. One approach would be to assume similar levels to Korea will emerge because high levels of incidence have been reported, despite the fact that just 25% of the population has undergone opportunistic ultrasound screening.9 This suggests that the levels in Korea could climb even higher, so using the current rates for pricing purposes may underestimate the potential future risk.
An alternative method of assessing the potential level of undiagnosed disease in the population is to study the prevalence of undiagnosed thyroid cancer found at autopsy in those without known disease. Harach et al. (1985) reported a prevalence rate of 35% for occult PTC at autopsy when thyroid glands were sectioned at 3-4 millimetres (mm) intervals.10 A more recent meta-analysis has demonstrated a 7.6% prevalence rate for PTC in over 7,800 autopsies with a sampling interval that varied between 1mm and more than 3mm.11 With modern ultrasound, lesions as small as 1mm in diameter have been identified and biopsied, so it is possible that a large reservoir of undetected thyroid lesions may exist and could still be diagnosed in the population.12 A weakness of these studies is that autopsy is more common with increasing age, whereas the incidence of PTC, illustrated in Figure 2, decreases with age in females.
Small-sized, early stage PTC constitutes the major part of the overall increase of thyroid cancer amongst all ages, but especially in women aged 30 to 60 years, yet worsening mortality has not been seen.13 Lesions described as microcarcinomas have an excellent long-term survival rate of over 95%.
Currently undetected thyroid cancers found by increased screening would satisfy many current CI definitions. To identify these tumours in the population does not require a step-change in technology because the equipment needed is commonly available and widely used. The cost of a simple non-invasive ultrasound scan is out of proportion to the potential CI claim benefit. Treatment is with surgical removal of part, or the entire, thyroid gland. Subsequent replacement medication may be necessary, but this is hardly a major life-threatening illness compared to many advanced cancers, strokes or progressive neurological disease.
Already most CI policies exclude early prostate cancer, non-melanoma skin cancers and certain indolent Chronic Lymphatic Leukaemias. These exclusions were introduced when the projected incidence rates threatened to drive up CI prices. If companies wish to guarantee the price of CI for any significant period, an exclusion of small PTC from the cancer definition may be a reasonable adjustment. In the Korean market, most CI products originally excluded PTC of less than 2 cm in size, but some of the larger companies have since completely excluded thyroid cancer from coverage.
The sharp rise in PTC diagnosis in Korea is likely to be replicated elsewhere. Those working on the design and pricing of CI may wish to consider an appropriate response. If the exclusion approach used in Korea is not followed, it could prove difficult to guarantee future CI risk in countries where similar levels of PTC incidence look likely. The Korean experience serves to highlight how new developments in screening can affect cancer incidence and therefore the cost of CI cover. There remains an interesting dichotomy between the possible benefits to patients of screening and the impact on providers of an insurance product that is diagnosis-based.

Segment Chief Underwriting Officer and Senior Medical Officer
See All Articles



