-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Biometric Information Privacy – Statutes, Claims and Litigation [Update]
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves?
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Illinois Changes Stance on Construction Defect Claims – The Trend Continues
Publication
Generative Artificial Intelligence in Insurance – Four Aspects of the Current Debate
Publication
Battered Umbrella – A Market in Urgent Need of Fixing -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Underwriting High Net Worth Foreign Nationals – Considerations for U.S. Life Insurance Companies
Publication
Group Term Life Rate & Risk Management – Results of 2023 U.S. Survey
Publication
Trend Spotting on the Accelerated Underwriting Journey
Publication
All in a Day’s Work – The Impact of Non-Medical Factors in Disability Claims U.S. Industry Events
U.S. Industry Events
Publication
Marginal Gains in the Medicare Supplement Market -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Sugar – The New Tobacco?

November 09, 2014
Ross Campbell
English
Obesity is a multi-factorial condition and the over-consumption of energy (calories) as sugar is a significant contributor to weight gain. When people take in more energy than they actually use up by body metabolism and physical activity, they create an imbalance. Sustained energy imbalance leads to an accumulation of excess body fat and weight gain over time.
The amount of added sugar in food and drink is of concern to scientists and government policy makers. Added sugars – which do not occur naturally – are increasingly blamed as the fuel of increasing obesity.1 It is added sugars that contribute additional calories, but zero nutrients, to our food. One reason for the popularity of sugary food and drink is that people have an innate preference for sweet tastes, although the degree varies individually.2
The World Health Organization has called for restrictions on sugar-sweetened beverages, even including taxation.3 Norway already taxes refined sugar products and Mexico introduced a “soda tax” in 2013. The last “Sugar Act” enacted by the British in 1764 raised taxes to defray the military cost of protecting its American colonies and to reduce treasury losses from smuggling. This unpopular legislation is regarded by historians as a tipping point toward the American Revolution. Perhaps those calling for a new tax on sugar hope it will herald revolution of a different sort?
For people whose weight has spiraled out of control, attempts to control and lose it by conservative means – dieting and exercise – are mostly ineffective. Increasing numbers of eligible people are therefore undergoing gastric bypass surgery. While there are undoubted improvements in vascular risk factors in people who sustain weight loss after bariatric surgery, it is no “silver bullet” cure for obesity.
Upsizing
Obesity is a major public health problem because of its association with diabetes, hypertension and hyperlipidaemia – themselves major risk factors for cardiovascular disease and cardiovascular-related mortality. Obesity is associated with cancer, disability, reduced quality of life and premature death.4 The international classification of body fatness defines “obesity” as a body mass index (BMI) of ≥30kg/m2.5 An individual is considered to be morbidly obese if he or she is 45 kilos over his or her ideal body weight, or has a BMI of 40 or more (35 or more if the individual has an obesity-related health condition).
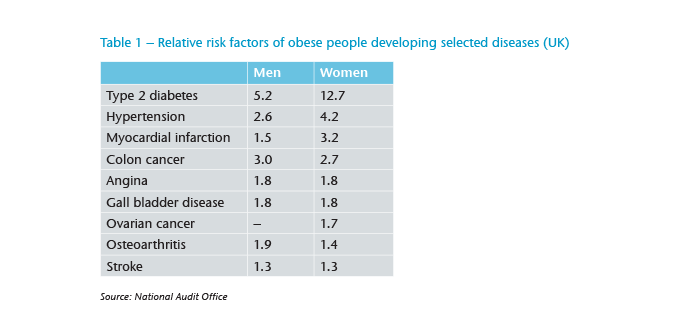
Evidence for the increasing prevalence of obesity is stark. For example, in England there was an increase from 13.2% of obese men in 1993 to 24.4% in 2012 and from 16.4% of obese women to 25.1% in the same period.6 About 6% of deaths in the UK are attributable to obesity and the risks associated with it are high (see Table 1).
Behavioral, societal and cultural factors underlie the global trend for people to get fatter. Cars, computers and calories form the basic ingredients of the obesity recipe. Contemporary lifestyles are often inactive with sedentary work patterns, modern technologies that simplify homemaking, and pastimes and activities that involve little or no exercise. Fundamental changes to work, transportation, leisure and food have exposed an underlying biological tendency for many people to unavoidably gain and retain weight. The post-war generation, reared on scarcity and rationing, has done rather well from an obesity perspective, but the baby-boomers much less well. Successive generations have enjoyed more luxurious lifestyles and an abundance of food, at least in developed countries. Advertising and cheap, fast, processed food, in large portion sizes or even super-size all play their part. The export of these irresistible delicacies to developing nations has fueled a rapid obesity increase in individuals unused to a high-fat-high-sugar diet.
It would be inaccurate, however, to explain all obesity by gluttony or laziness. Genes can have a strong influence, affecting the method and the location of fat storage in the body, and the family environment is a factor because families share food and physical activity habits. Hormonal problems including hypothyroidism, Cushing’s syndrome and polycystic ovarian syndrome are associated with overweight tendencies. Certain medicines prompt weight gain as they slow the metabolic rate, increase appetite and cause water retention. Pregnancy causes natural weight increase and this can prove hard to lose for some, while menopause adds weight and alters body fat distribution. A lack of sleep disrupts the balance of hormones – ghrelin (hunger) and leptin (satiety) – and affects how the body reacts to insulin, thus pushing up blood sugar levels. People can overeat when they quit smoking or are bored, angry or stressed. Those who cannot reduce their calorific intake with age will gain weight as their exercise levels drop. These factors do not absolve all personal responsibility but many people have found themselves simply overwhelmed by the multiple forces that drive obesity.
Downsizing
It is simple to calculate the number of calories per serving, as 1 gram of sugar is equivalent to 4 calories. Any processed, sweetened product without fruit or milk ingredients contains only added-sugars. It seems unfeasible that anyone would add nine teaspoons (35g) of sugar to a glass of cola to make it palatable, yet a 330ml can contains this amount of added-sugar. If consumers had to add the sugar themselves, no doubt they would put in less.
A “rule of thumb” reference maximum daily intake for adults of 90g of total sugar has been in place across the EU since 2006.7,8 Current UK government advice says no more than 11% of a person’s daily food calories should come from added sugars (or 10% taking alcohol into account), which equates to a daily intake for women of 50g and for men of 70g. However, people of all age groups are eating much more sugar than the recommended 11% level, prompting a review of dietary recommendations on carbohydrates, including advice on sugar.9
People at risk of becoming obese or who are already overweight are advised to exercise at moderate intensity for up to 300 minutes every week. Eating low-calorie, nutrient-dense foods, such as fruits, vegetables and whole grains, while avoiding saturated fat and limiting sweets and alcohol are recommended. Interestingly, rapid or fad dieting is not recommended by clinicians. Alternatively, people are advised to plan their food intake, to avoid situations where their eating becomes uncontrolled, to monitor their weight regularly and to adhere to these revised behaviours on a consistent basis.
The simple solution seems to be to eat less and exercise more. Yet there are difficulties with over-simplification of this complex matter. Although exercising burns stored calories, the idea that the benefits of exercise are primarily derived from the number of calories burned is scientifically inaccurate.10 High-intensity bursts of interval training provides equal, or better, aerobic benefits than prolonged low- or moderate-intensity exercise that consumes the same number of calories.11
Resizing
Gastric bypass is a surgical procedure that isolates the upper part of the stomach, below the esophagus, to create an egg-sized pouch that has about 25% of the capacity of a normal stomach. The pouch is then connected to the jejunum. Food bypasses the stomach and an unused portion of duodenum and goes directly into the small intestine. The intended effect of this surgery is to limit fat and calorie absorption.
Following gastric bypass patients must learn to eat differently. Food must be chewed slowly up to 20 or 30 times to make it smooth before it is swallowed to avoid blocking the pouch. Not all food types can work in this approach – rice for example – with the result that many food favorites are struck from the menu. Switching to low-fat protein menus can prove a challenge. Changes to established rituals and social pleasures of eating meals that are necessary to ensure compliance with the post-surgery regimen simply prove too difficult for some.
Gastric surgery does not alter the way people metabolise calories. They can gain weight if they consume food that has a high calorie-to-volume ratio. The relationship some people have with food can work against a successful outcome – their desire to lose weight overruled by biological hunger. Many prior habits, feelings and attitudes towards food remain unchanged – for example the urge to eat high-calorie foods. In the months after surgery patients may endure hair loss, nausea, palpitations, dumping syndrome, low mood and depression. It is prudent for underwriters to postpone applications made in the first 12 months following surgery as the post-operative complication rate falls and the success of the procedure can be better judged.
There are undoubted improvements in many vascular risk factors in people who lose weight with bariatric surgery – diabetes, hyperlipidaemia, hypertension and sleep apnoea have been observed to improve or resolve.12 The key question is whether bariatric surgery “heals” any metabolic disease associated with obesity; effectively wiping the risk slate clean. The evidence available currently suggests that it does not.
Median survival is reduced by 2 to 4 years by a BMI of 30 - 35. BMI 40 - 45 reduces it by 8 to 10 years.13 The short-term resolution of vascular risk factors following gastric bypass translate into small improvements in long-term mortality – no more than 3 years – with the absolute life expectancy benefit similar across age groups.14,15 The progressive excess mortality is due mainly to vascular disease. The effect of depression in the severely obese may not be resolved by surgery and any subsequent loss of weight.16 Depressive disorders after surgery significantly predict reduced weight loss.17 There is an increased rate of suicide in those who have undergone bariatric surgery.18
It is over-optimistic to suggest that people who lose weight (to a level not normally rated by underwriters) this way are standard risks for life insurance. There is a long tail risk from the surgery, psychological issues and more especially the vascular damage that will have occurred during the time risk factors were elevated by obesity. Although the degree and persistence of this elevated risk can be argued, an extra rating is appropriate for individuals who have undergone bariatric surgery.
Summarizing
The information provided on food packaging may be confusing, or even deliberately obfuscated by manufacturers, but portion size is within the control of everyone. Fast food and take-away establishments can be avoided. Exercise can be taken. The problem for policymakers seeking to tackle the growing trend towards obesity using a “healthy eating” or “energy balance” message is that real change demands people alter entrenched shopping, eating, home, family and leisure habits. Challenging the psychological ambivalence of individuals who have made lifestyle choices that may have led to inevitable obesity will not be easy. Stark health warnings and government campaigns about healthy eating face stiff competition from primary appetite control mechanisms in the brain and the force of dietary habit. Tobacco again proves an unlikely parallel for excess sugar-risk; despite dire health consequences, high taxation and use restrictions, many people continue to smoke.
The arguments over preventable deaths and excess consumption of added sugar sound similar to those around tobacco control. In a close parallel with tobacco companies’ reaction to the commercial threat of e-cigarettes, the food industry giants fear losing out to products from small, independent companies that have a greater health focus. So far, the food and drinks industry has avoided extra regulation through voluntary deals – mainly reducing the volume and weight of individual products. Many of the claims for reduced sugar (and fat) content in products therefore come from the manufacturers themselves. As the clamour to do something positive to limit obesity intensifies, governments facing escalating healthcare costs could opt to impose taxes or regulation to force changes in eating habits.
The physiological mechanisms triggered by bariatric surgery, which physically reduces calorific capacity provoking rapid weight loss in some patients, offer further clues to the complexity. Rather than stemming from pure calorie limitation, any weight loss following surgery may in fact result from changes to insulin, ghrelin and leptin levels and the action these hormones have on multiple systems, including the brain, muscles and fat.19 Setting aside poor compliance with the strict eating regimens required for surgery to prove successful, increased physical activity and reduced calorie intake alone would not appear to guarantee weight loss.




