-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Structured Settlements – What They Are and Why They Matter
Publication
PFAS Awareness and Concern Continues to Grow. Will the Litigation it Generates Do Likewise?
Publication
“Weather” or Not to Use a Forensic Meteorologist in the Claims Process – It’s Not as Expensive as You Think
Publication
Phthalates – Why Now and Should We Be Worried?
Publication
The Hidden Costs of Convenience – The Impact of Food Delivery Apps on Auto Accidents
Publication
That’s a Robotaxi in Your Rear-View Mirror – What Does This Mean for Insurers? -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Key Takeaways From Our U.S. Claims Fraud Survey
Publication
Favorite Findings – Behavioral Economics and Insurance
Publication
Individual Life Accelerated Underwriting – Highlights of 2024 U.S. Survey
Publication
Can a Low-Price Strategy be Successful in Today’s Competitive Medicare Supplement Market? U.S. Industry Events
U.S. Industry Events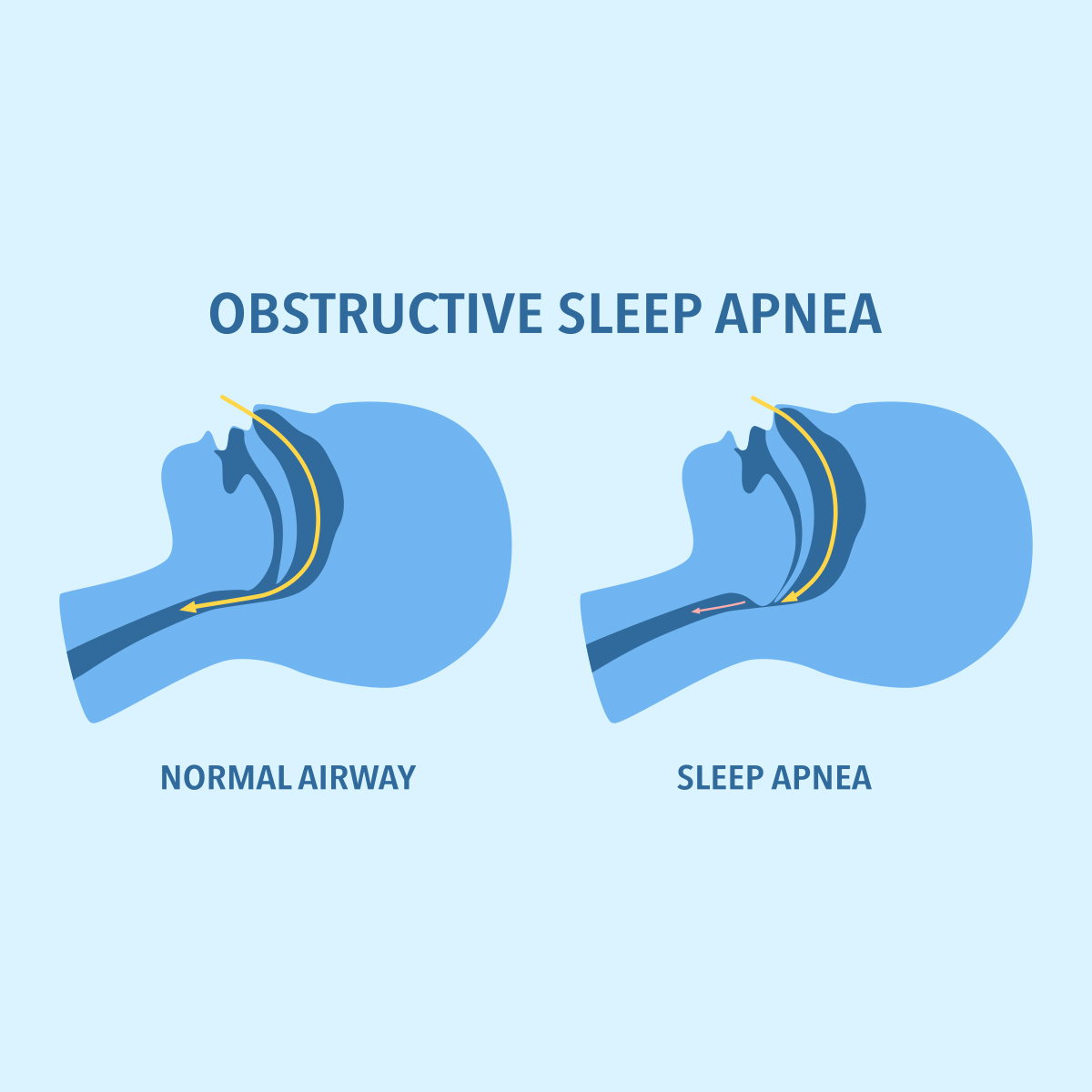
Publication
The Latest in Obstructive Sleep Apnea -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Long-COVID – What Are the Long-term Effects of COVID-19?

One year after the outbreak of COVID‑19, it has become apparent that patients who have recovered from the acute illness may still struggle with long-term consequences. Although a negative PCR test confirms that acute viral infection is no longer present, the effects on the immune system and inflammatory processes in the body can persist and lead to long-term symptoms even in previously mild and asymptomatic COVID‑19 cases. Therefore, it can be assumed that a considerable number of people are officially recovered but still affected.
Patient surveys taken weeks to months after a COVID‑19 diagnosis primarily point to the following long-term symptoms:
- Shortness of breath
- Concentration problems
- Forgetfulness
- Memory loss
- Disturbances of the sense of smell and taste
- Tiredness and exhaustion
- Mood swings
- Muscle and joint pain
This symptom pattern, also described as “Long-COVID”, is manifested to varying degrees of severity. Fluctuating strength or the disappearance and later recurrence of symptoms are also reported.1
For underwriting, a holistic approach based on the risk assessment triangle is recommended. In order to be able to make an adequate risk assessment, it is necessary to determine the current state of health and the requirements at work and during leisure activities. Therefore, an overview of the many faces of Long-COVID is required: How often and how seriously do symptoms occur, how long do they persist and what is the underlying cause?
Breathing difficulties
SARS‑Cov‑2, the name of the COVID‑19-triggering virus, stands for Severe Acute Respiratory Syndrome Corona Virus‑2, which indicates that the respiratory system is the first to be affected. Typical consequences are the so-called ground-glass opacities of the lungs that are detected by CT. They initially describe areas of lung consolidation. In COVID‑19, this is caused by an inflammatory leakage of blood components from the capillaries and a local accumulation of fluid. This hinders the exchange of oxygen from the lungs into the blood and induces symptoms, such as shortness of breath and coughing.
Ground-glass opacities have also been detected in asymptomatic patients and those with only mild COVID‑19.2 The conditions under which the ground-glass opacities regress or develop into persistent complaints and fibrosis have not yet been sufficiently investigated. Fibrosis describes a scarring and hardening of the connective tissue between the pulmonary alveoli and blood vessels, which can permanently disrupt the exchange of oxygen. So far, the development of fibrosis has been reported mainly in severe cases.3
Mild disease can manifest with significant lung involvement. Even in clinically healthy divers who recover from it, follow-up checks after infection revealed ground-glass opacities, a lack of gas exchange between lung and blood (lung shunt), reduced oxygen saturation and bronchial hyperexcitability.4 Based on these findings, a diving suitability test is no longer considered valid after a COVID‑19 infection and the diver should be re-certified afterwards. In a statement, the German Society for Diving and Hyperbaric Medicine (GTÜM), the Medical Director of the German Life Saving Society (DLRG), and the Medical Department of the German Sports Divers’ Association (VDST) have agreed on this.5,6
Persistent lung damage especially poses a risk for physically demanding jobs and activities. Some examples include soldiers, construction workers, police officers, professional/leisure divers, firefighters and athletes.
At present, however, it has been shown that ground-glass opacities usually regress and recover over time. The results of the Austrian CovILD study show a decrease in lung damage within several months.7,8 Six weeks after discharge from hospital, 88% of the patients still had visible lung damage on CT and 65% reported shortness of breath. Twelve weeks later, 18 weeks after discharge, these figures dropped to 56% and 39% respectively. Similarly, lung function values improved. Initially one-third of patients had abnormal values and this reduced to one-fifth. Ground-glass opacities were more frequently detected than respiratory distress or restrictions in the lung function tests. Therefore, ground-glass opacities do not necessarily lead to noticeable symptoms in everyday life. Due to the likely improvement over time, a new risk assessment of the lung function can be offered at a later stage.
Organ damage
During the acute infection, further organ damage may occur. Most frequently observed were:
- Heart damage9 (myocardial injury, arrhythmia, acute coronary syndrome, myocarditis)
- Loss of renal function (acute kidney damage, which can develop into chronic kidney disease)10,11,12,13
- Brain damage14,15 (stroke, cerebral hemorrhage, encephalitis)
Possible causes of this are an overreaction of the immune system with increased cytokine release as well as inflammation of the vessel walls leading to coagulation disorders. This can lead to hemorrhages or clots, which interrupt the blood supply and cause tissue damage.16,17,18
In addition, the virus uses ACE2 receptors to penetrate the target cells.19,20,21 In acute infections, higher ACE2 receptor levels in individual organs can also lead to a higher susceptibility to more severe local infections.
In the case of persistent symptoms (Long-COVID), the overactive immune system may be responsible for continuing inflammatory processes. Possible explanations for this are residual viral foci in individual organs that are not detected by nasal/pharyngeal swabs, fragments of the viruses that can no longer replicate but continue to be fought by the immune system, or a persistence of the immune system in an overactive state,22 as observed in the case of Infectious mononucleosis (glandular fever).
Therefore, an increased risk for the development or aggravation of secondary damage could also persist in the long term. For further clarification, several programs were initiated in June by the British Heart Foundation to assess both the acute and long-term risk of cardiovascular complications and multi-organ damage from COVID‑19.23
Sensory & nervous system
Another early symptom of the disease is the loss of the perception of smell and taste.24,25 The taste buds of the tongue usually recognize five tastes – salty, sour, bitter, sweet and savoury/meaty (umami). A more complex taste picture always depends on the perceived odours of a dish. Whether COVID‑19 changes the taste reception in the mouth or causes this impression by a reduced olfactory perception due to olfactory nerve inflammation cannot yet be answered.
Primarily this is relevant for the professions of cook, perfumer, sensory analyst, olfactory examiner as well as further professions in which taste and olfactory perception are essential. This should be considered individually, especially since these sensory complaints are often not included in the standard health questions.
How often do olfactory and gustatory restrictions occur after an illness?
A survey of 4,039 COVID‑19 patients at Forschungszentrum Jülich showed that 80% of them suffered a loss of olfactory ability and 70% a reduction in taste perception. In the majority of cases, the loss was complete and often lasted three months after the illness.26 A survey of 102 patients conducted by UC San Diego Health showed similarly high values of 68% olfactory and 71% gustatory-affected patients. However, 74% of the patients experienced a decrease in symptoms within two to four weeks.27 A prospective study of 202 mild COVID‑19 cases showed in 41% an improvement and in 49% a complete recovery four weeks after the onset of the disease. In only 11% of the cases did the symptoms persist unchanged.28 Since the complaints decrease over time, a deferral for a short period may be sufficient in cases of occupational relevance.
If long-term complaints remain, a decrease in appetite and resulting weight loss could be a possible complication, which needs to be evaluated individually.
The extent to which other sensory functions, such as vision and hearing, are affected has not been conclusively examined. In 1%‑5% of the cases, COVID‑19 infection leads to acute conjunctivitis, which is not expected to lead to subsequent complications. However, there are also some case descriptions in which both microhemorrhages and cotton wool stains caused by capillary occlusion of the retina occurred.29,30 In two case descriptions so far, paracentral acute intermediate maculopathy (PAMM) and acute macular neuroretinopathy (AMN) have been described, which may lead to retinal atrophy and impaired vision in the long-term.31 Effects on hearing up to unilateral hearing loss with subsequent improvement have also been observed in asymptomatic patients.32,33
According to the recent data, the risk of long-term vision and hearing loss appears to be rather low.
Mental health
The psychological effects of an illness are difficult to classify. For example, health problems, hospital and intensive care treatment, a life in quarantine and isolation, stigmatization as a sick person, and fears about the illness, recovery and economic consequences can be very stressful. This can manifest in the form of sleep disorders, depression, anxiety, obsessive-compulsive disorders and post-traumatic stress disorders, or it can aggravate already existing mental and physical illnesses.34
For example, a look at long-term SARS studies shows that 42.5% of patients still suffered from mental disorders 2.5 to 4 years after their release, while only 3.3% had a mental illness before. The most frequent diagnoses were post-traumatic stress disorder (54.5%), depression (39%), somatoform pain disorders (36.4%), panic disorders (32.5%) and obsessive-compulsive disorders (15.6%).35 However, SARS much more frequently led to severe disease courses than COVID‑19. Consequently, more intensive care treatment was needed, a course that further increases the probability of psychological secondary diseases.36,37 For COVID‑19, with around 80% being mild cases, a lower rate of affected persons can be assumed.38
Exhaustion, muscle & joint pain
The most frequently described consequences of COVID‑19 disease are fatigue and exhaustion.39,40 In a French study of hospitalized COVID‑19 patients, 55% still suffered from exhaustion 3.5 months later.41 In another survey, 35% of young, previously healthy adults with a mild course of the disease still showed persistent fatigue two to three weeks later.42 Some case reports describe persistent severe fatigue that makes it impossible to fulfill the previous job and everyday duties.43 The symptoms are similar to the controversial diagnosis of myalgic encephalomyelitis (ME), also known as chronic fatigue syndrome. For ME, the underlying causes are still not fully resolved.44 Possible explanations include a dysregulated immune system, autoimmune-responses and physical/psychological stress.45 Consequently, the various treatment approaches have uncertain success.
The existence of ME as a diagnosis is still controversial. The partial lack of medical and social recognition often leads to further frustration among those affected.
In comparison, long-term studies of SARS patients showed that 40% still suffered from chronic exhaustion 3.5 years later; 27% of them fulfilled the criteria of chronic exhaustion syndrome at that time.46
To what extent the same post-COVID symptomatology with numerous patients worldwide can contribute to resolving ME remains to be seen. However, the risk of prolonged chronic exhaustion should be considered, especially in the case of occupation-related and Disability products.
Memory loss and concentration disorders
Another symptom is the so-called “brain fog” or thought disturbances that can manifest in the form of memory loss and concentration disorders.47 Both complaints can also occur in the context of ME.
A French study of hospitalized COVID‑19 patients showed that 3.5 months later, 34% still suffered from memory loss and 28% from concentration problems.48 Again, patients with a previously mild disease course were affected, too. Some people describe dementia-like conditions that make it significantly more difficult or even impossible to carry out their previous job and normal self-care in everyday life and that can last for more than six months.49,50,51 Possible explanations for this are, again, an infection of nerve cells/brain, a permanently increased immune defense as well as autoimmune reactions, through which the immune system attacks the patient’s nerve cells.52,53 These symptoms are particularly relevant for the assessment of occupational and basic skills products, which include intellectual abilities.
Metabolic changes
Several studies indicate that COVID‑19 can lead to elevated blood glucose levels and might promote metabolic disease.54,55,56,57,58 SARS‑Cov‑2 infection has been shown to damage pancreatic cells.59,60,61 Consequently, an increased risk for the development of diabetes as well as for the aggravation of pre-existing diabetes is assumed.
In contrast, blood lipids appear to decrease in the course of acute, severe COVID‑19 disease, so that hypolipidemia is also considered a risk factor for a severe acute course.62 In this context, the molecule SREBP2 appears to interfere with cholesterol synthesis and to promote a cytokine storm.63
The presence of other symptoms – such as breathing difficulties, pain, exhaustion and mental health problems – will further reduce exercise and daily movements; this can amplify the development of metabolic disease.
Whether COVID‑19 increases the risk of metabolic diseases in the long-term, and whether only glucose metabolism is affected by it, cannot yet be conclusively assessed. To help define these issues, the international database COVIDIAB was created, which records the incidence of diabetes during and after COVID‑19 infection as well as the further course of existing diabetes.64
Follow-up examinations of SARS patients also indicate an increased long-term risk of lipid and sugar metabolism disorders; 12 years after the disease, 68% suffered from hyperlipidemia and 60% from abnormal glucose metabolism, while in the control group only 40% and 16% were affected.65
Prognosis factors for Long-COVID – Who is at risk?
The COVID Symptom Study App provides a first overview of who is more likely to develop Long-COVID after an acute infection. More than four million users have described their post-COVID symptoms here.
The first published evaluation of slightly more than 4,000 participants showed that one in 22 COVID‑19 cases is still affected by Long-COVID symptoms eight weeks later; every 44th person maintains symptoms after four more weeks.66
Risk factors identified here are an increased BMI and higher age, although any age group can be affected. In the younger age group, the risk for women seems to be higher than for men. Since males have a higher risk of a severe acute COVID‑19 disease, this raises further questions about the underlying differences. For Long-COVID, there may be a connection with the fact that chronic fatigue syndrome occurs more often in women than in men.67 Asthma is another risk factor for Long-COVID. In general, the probability for Long-COVID increased with the number of symptoms in the first week.
However, it should be noted that the survey results are self-declarations and patients with persistent symptoms are more likely to participate in this survey. Therefore, the actual numbers may be lower.
The WHO recently declared increased blood pressure, overweight and psychological complaints as possible risk factors for Long‑COVID.68
Studies on the occurrence and course of Long-COVID
In order to investigate on a broad basis how frequently and under what circumstances Long-COVID occurs and how long the symptoms persist, several large-scale long-term studies and surveys have been launched.
Examples:
- PHOSP-COVID – The Post-Hospitalization COVID‑19 study69
- COVIDOM UKSH long-term study over 1.5 years70
- Covid Symptom Study App Survey71
- COVIDIAB Diabetes Database: Prevalence before and incidence after COVID‑1972
- Several programs of the British Heart Foundation for cardiovascular complications and multi-organ damage during and after COVID‑1973
Is there immunity after COVID‑19 disease?
Recovery from COVID‑19 disease also raises the question whether a reinfection is now less likely. Currently, there are four documented cases of reinfection between 1.4 and 4.5 months after initial infection.74 Two of these cases showed milder symptoms at reinfection and the few case reports in relation to the global total number of cases indicate usually at least an attenuating immune response on secondary COVID‑19 infections. In general, however, reinfection cannot be ruled out, and in two case reports, the second infection even led to a more severe course than before.75 Therefore, it is not recommended to assume immunity after recovery and to consider a continued susceptibility to COVID‑19.
In general, antibody levels and the duration of sufficiently elevated antibody levels appear to scale with disease severity and, depending on the study, may be detectable from less than two months to at least seven months after infection.76,77 The average duration of immunity, and the extent to which it is maintained by T and B memory cells in the long-term,78,79 requires broadly based follow-up studies for years after infection, which are not yet available for this young disease.
Outlook
In summary, the post-COVID‑19 symptoms observed so far have also been described with other viral diseases. To what extent the long-term prognoses of the other coronavirus diseases SARS and MERS can be transferred to COVID‑19 cases cannot be answered at present, especially since significantly fewer people were affected at that time and the course of the disease was often more severe. Since COVID‑19 has only been described since December 2019, long-term studies over several years are not available. Until then, a Long-COVID patient’s risk can only be assessed based on an individual’s present complaints; prognoses from other viral diseases should serve as references.
Since we know that SARS‑Cov‑2 is spreading rapidly, that more than 90 million cases are already known worldwide,80 and that even mild infections can have long-term effects, we will increasingly have to face the holistic risk assessment of Long-COVID complaints. The symptoms described here are therefore intended to provide an initial overview and are based on the findings to date, which can certainly be further supplemented and refined over time.81
At present, it is advisable to postpone assessment during the acute phase of COVID‑19. Afterwards, the initial and remaining symptoms need to be carefully assessed. Prognosis of other viral disease long-term effects can serve as reference. The symptom significance should be classified product-specifically (what is covered?) and in relation to the risk assessment triangle (health status of the applicant and current professional and leisure requirements).
Based on the current state of research, a prognosis can be made, possibly in consultation with a physician. If a prognosis about the further course of the disease cannot be made at present, a wait-and-see approach with a deferral is recommended.





