-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Structured Settlements – What They Are and Why They Matter
Publication
PFAS Awareness and Concern Continues to Grow. Will the Litigation it Generates Do Likewise?
Publication
“Weather” or Not to Use a Forensic Meteorologist in the Claims Process – It’s Not as Expensive as You Think
Publication
Phthalates – Why Now and Should We Be Worried?
Publication
The Hidden Costs of Convenience – The Impact of Food Delivery Apps on Auto Accidents
Publication
That’s a Robotaxi in Your Rear-View Mirror – What Does This Mean for Insurers? -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Key Takeaways From Our U.S. Claims Fraud Survey
Publication
Favorite Findings – Behavioral Economics and Insurance
Publication
Individual Life Accelerated Underwriting – Highlights of 2024 U.S. Survey
Publication
Can a Low-Price Strategy be Successful in Today’s Competitive Medicare Supplement Market? U.S. Industry Events
U.S. Industry Events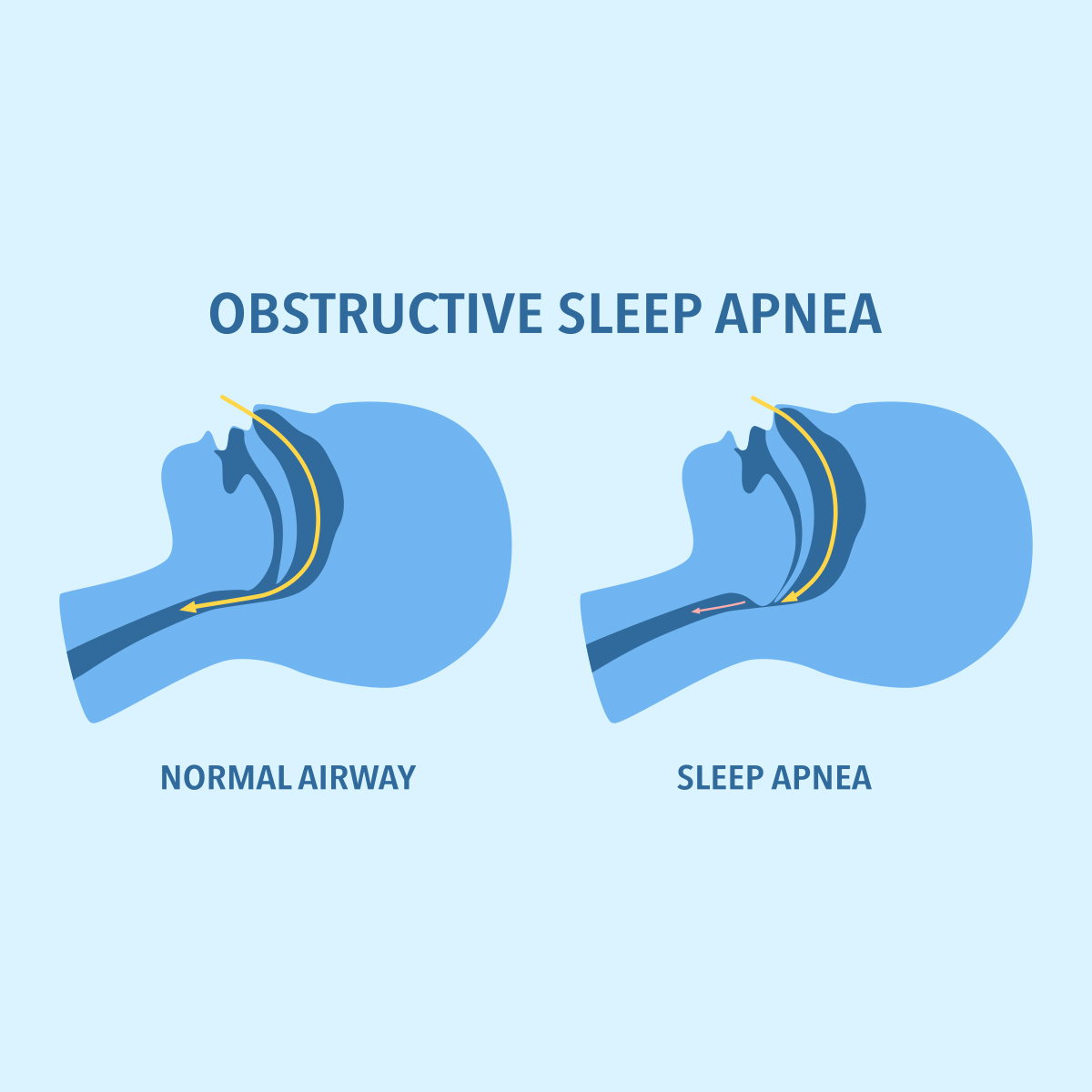
Publication
The Latest in Obstructive Sleep Apnea -
Knowledge Center
Knowledge Center Overview
Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Why Do Some People Survive to Age 100? - An Actuary’s Perspective

May 29, 2019
Beata Puls
English
Deutsch
Developing reliable life tables is one of the most important objectives for life insurance companies. Mortality rates for single ages are usually very small numbers and we need a rather large sample size to obtain reliable estimates. Otherwise, they are too sensitive to small changes in the number of death cases. This is often a problem when it comes to estimating mortality in very high ages. From an actuarial perspective, it is a challenge that an individual dies only once.
In middle age, when the probability of death is roughly 1 per mille, an actuary would need more than 20,000 person-years to derive reliable mortality rates. This is usually not an issue since this is the core age range for policyholders of life insurance products. But for both genders in high ages, we observe a rapid reduction in the lives exposed and therefore the number of death cases (see chart). Although mortality rates increase nearly exponentially with age, there is a rapid drop in death cases for males above age 85 and above age 90 for females. A similar pattern is observed for many populations.

Understanding the uncertainty around mortality and risk profiles in advanced ages is of crucial importance for life insurance companies. Family studies show that genetic factors can explain 20%-30% of the variation in longevity, whereas most of the remaining variation is attributed to environmental effects.
Two Recent Studies
1 - Assessing the Prevalence of Morbidity in Long-Lived Individuals
Recently, a team working with Gabriele Doblhammer at the University of Rostock in Germany assessed the prevalence of morbidity at extreme old ages. Doblhammer’s team used health claims data from AOK, a large German public health insurer, and compared two birth cohorts. The older cohort was followed from age 95 until death or survival to age 100 and the younger one from age 85 to 90. Based on data for almost 20,000 insured lives, they analyzed how individuals who survived to very high ages differ from the remaining population with respect to the diagnosis of certain diseases.
For the older cohort, the most common diagnosis was the residual group of other chronic heart diseases - such as cardiomyopathy, heart failure and rheumatic heart disease - and the second most common was dementia, with a prevalence of 59% and 53% respectively. Moreover, 73% in this group had hypertension and 30% had diabetes, which were both much more prevalent in the younger cohort. For all diseases studied, prevalence continued to increase with age. However, long-lived individuals had significantly lower prevalence at each age.
When differentiated according to age at death, greater longevity was significantly associated with a lower prevalence of dementia and chronic heart diseases. Of those who survived past the age of 100, 28% had dementia at age 95 and this increased to 54% at age 100. These trajectories of prevalence by age increased for individuals who died at younger ages. In the group of those who died between the age of 97 and the age of 99, the highest prevalence of dementia reached almost 70% before death, which is significantly higher than in the long-lived individuals who survived to age 100. Among those who died at age 95, the prevalence of dementia was already 55%. A similar pattern of trajectories was observed for other chronic heart diseases, although it was less distinct than for dementia. The lower prevalence of dementia and chronic heart diseases among those who lived longer was also clearly seen in the younger cohort.
In contrast to these observations, for other common conditions, such as hypertension or diabetes, there was no clear link between the prevalence and the age at death in the older cohort. There was no survival advantage for centenarians compared to their cohort for hypertension, and only small advantages for nonagenarians. For diabetes the effect was more pronounced in the younger cohort.
2 - Assessing the Association Between Body Size and Physical Activity With Longevity
At the Maastricht University Medical Center in the Netherlands, research undertaken by Lloyd Brandts focused on body size and physical activity and their association with longevity. This team analyzed the likelihood of reaching 90 years of age with respect to height, body mass index (BMI), change of BMI since age 20, and non-occupational physical activity for the oldest birth cohorts in the Netherlands Cohort Study (NLCS), which were aged 68-70 years at baseline. They found notable differences between survival patterns in males and females.
For females a significant influence of height and BMI were identified for reaching longevity. Females taller than 175 cm had a 31% higher chance of reaching the age of 90 compared to females shorter than 160 cm. Compared with normal weight females, obese females that had a BMI greater than 30 showed a 32% lower chance of reaching longevity. Furthermore, an increase in BMI since age 20 of more than 8 points was associated with a 19% lower probability to live to high ages compared with females who gained less than 4.
For males, body height or size did not play a role in reaching longevity, but rather the level of physical activity at the age of 60. Males who reported more than 90 minutes of physical activity per day were almost 40% more likely to reach high ages than those who reported a low level of physical activity. For females the optimal range of physical activity was a medium level, between 30 and 60 minutes per day, and the likelihood of reaching longevity did not change significantly for higher levels of exercise. For men and females, no significant associations were found between BMI at age 20 and reaching longevity.
Our Thoughts
In line with these findings, we observe an increased interest in continuous monitoring of health and lifestyle factors of the insured population, such as the changes in BMI over time and the level of physical activity. Especially with the increasing prevalence of obesity around the world, the impact of healthy behavior on life expectancy becomes more relevant. In the future, life insurance companies might use this information to differentiate their premiums or even adjust them on a continuous basis to increase customer engagement throughout the term of the policy.
Besides the traditional benefits, an insurer could offer targeted programs to decrease BMI or increase the level of physical activity in higher ages to improve their customers’ well-being and the chances of reaching longevity.
This blog originally appeared in our e-newsletter series “The Future of Old Age - Insights for Insurers.”
References
- Brandts, L., & van den Brandt, P. A. (2019). Body size, non-occupational physical activity and the chance of reaching longevity in men and women: Findings from the Netherlands Cohort Study. Journal of Epidemiol Community Health, 73(3), 239-249. doi:10.1136/jech-2018-211410.
- Doblhammer, G., & Barth, A. (2018). Prevalence of Morbidity at Extreme Old Age in Germany: An Observational Study Using Health Claims Data. Journal of the American Geriatrics Society, 66(7), 1262-1268. doi:10.1111/jgs.15460.